Colonoscopy
Test Overview
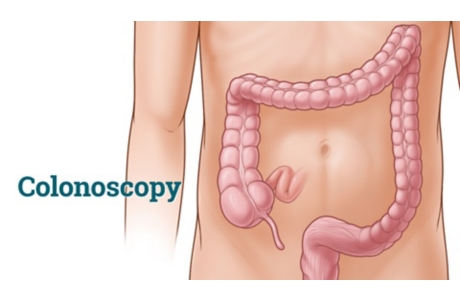
Colonoscopy is a test that allows your doctor to look at the inner lining of your large intestine (rectum and colon). He or she uses a thin, flexible tube called a colonoscope to look at the colon. A colonoscopy helps find ulcers, colon polyps, tumors, and areas of inflammation or bleeding. During a colonoscopy, tissue samples can be collected (biopsy) and abnormal growths can be taken out. Colonoscopy can also be used as a screening test to check for cancer or precancerous growths in the colon or rectum (polyps).
The colonoscope is a thin, flexible tube that ranges from 48 in. (125 cm) to 72 in. (183 cm) long. A small video camera is attached to the colonoscope so that your doctor can take pictures or video of the large intestine (colon). The colonoscope can be used to look at the whole colon and the lower part of the small intestine. A test called sigmoidoscopy shows only the rectum and the lower part of the colon.
Before this test, you will need to clean out your colon (colon prep). Colon prep takes 1 to 2 days, depending on which type of prep your doctor recommends. Some preps may be taken the evening before the test. For many people, the prep is worse than the test. The bowel prep may be uncomfortable, and you may feel hungry on the clear liquid diet. Plan to stay home during your prep time since you will need to use the bathroom often. The colon prep causes loose, frequent stools and diarrhea so that your colon will be empty for the test. If you need to drink a special solution as part of your prep, be sure to have clear fruit juices or soft drinks to drink after the prep because the solution may have a salty or unpleasant taste.
Colonoscopy is one of the many tests that may be used to screen for colorectal cancer. Other tests include stool tests, sigmoidoscopy, and CT colonography. Which screening test you choose depends on your preference. Talk to your doctor about what puts you at risk and what test is best for you.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Why It Is Done
Colonoscopy is done to:
- Check for polyps as a screening test for colorectal cancer.
- Check for the cause of blood in the stool or rectal bleeding.
- Check for the cause of dark or black stools.
- Check for the cause of chronic diarrhea.
- Check for the cause of iron deficiency anemia.
- Check for the cause of sudden, unexplained weight loss.
- Check the colon after abnormal results from a CT scan, MRI, virtual colonoscopy, stool test, or barium enema.
- Watch or treat inflammatory bowel disease (IBD).
- Check for the cause of long-term, unexplained belly pain.
How To Prepare
Before you have a colonoscopy, tell your doctor if you:
- Are taking any medicines, such as insulin or medicines for arthritis. Check with your doctor about which medicines you need to take on the day of your test.
- Are allergic to any medicines, including anesthetics.
- Have bleeding problems or take aspirin or other blood thinners.
- Had an X-ray test using barium, such as a barium enema, in the last 4 days.
- Are or might be pregnant.
You may be asked to stop taking aspirin products or iron supplements 7 to 14 days before the test. If you take blood-thinning medicines regularly, discuss with your doctor how to manage your medicine.
You will be asked to sign a consent form that says you understand the risks of the test and agree to have it done.
Talk to your doctor about any concerns you have regarding the need for the test, its risks, how it will be done, or what the results will mean. To help you understand the importance of this test, fill out the medical test information form( What is a PDF document? ).
Arrange to have someone take you home after the test, because you may be given a medicine (sedative) to help you relax before the test.
Colon prep
Before this test, you will need to clean out your colon. The following information gives you a general idea of the preparation for a colonoscopy. Your doctor will give you specific instructions before your test.
- One to two days before a colonoscopy, you will stop eating solid foods and drink only clear fluids, such as water, tea, coffee, clear juices, clear broths, flavored ice pops, and gelatin (such as Jell-O). Do not drink anything red or purple, such as grape juice or fruit punch. And do not eat red or purple foods, such as grape ice pops or cherry gelatin.
- Your doctor will recommend a medicine for you to use to prepare for your colonoscopy. It will most likely be a prescription laxative tablet and/or a laxative solution (such as Nulytely or Golytely) that you drink before your colonoscopy. This solution will be given to you as a powder that you will mix with 1 gal (3.8 L) of water. You may need to drink this laxative solution over 1 to 2 hours in the evening before the test. Or you may be asked to drink half the solution the evening before your test and the other half the morning of your test. This solution may taste very salty and may make you feel sick to your stomach. To make your colon prep easier, you may want to try some of the following tips:
- You may find it easier to drink the solution if you use a straw with the end at the back of your throat (to bypass the taste buds).
- Each time you drink some of the solution, you may also drink some water or clear fluids (like apple juice) to help get rid of any unpleasant taste in your mouth.
- Ask your doctor if it is okay for you to add flavored drink crystals (such as Crystal Light) to the solution.
- Add lemon juice to the solution or suck on sliced lemon wedges after you take a drink.
- You may find it easier to drink the solution if you chill it in the refrigerator first.
- Your doctor may recommend a different preparation product, such as the Nutraprep meal kit or sodium phosphate tablets (for example, Visicol). These are other methods of preparing for a colonoscopy. If you are concerned about the standard bowel prep, you can ask your doctor whether another method will work for you.
- Oral sodium phosphate (either tablets or liquid) can cause kidney problems. Make sure you check with your doctor before using a nonprescription sodium phosphate product.
- You will want to stay home while doing the colon prep, because the colon prep will make you use the bathroom often.
- Drink plenty of clear fluids during the prep so you will not get dehydrated. This will also help clean out your colon completely after you finish the colon prep.
- Do not eat any solid foods after doing the colon prep.
- Stop drinking clear liquids 6 to 8 hours before the colonoscopy.
How It Is Done
Colonoscopy may be done in a doctor’s office, clinic, or a hospital. The test is most often done by a doctor who works with problems of the digestive system (gastroenterologist). The doctor may also have an assistant. Some family doctors, internists, and surgeons are also trained to do colonoscopy.
During the test, you may get a pain medicine and a sedative put in a vein in your arm (IV). These medicines help you relax and feel sleepy during the test. You may not remember much about the test.
Before the test
You will need to take off most of your clothes. You will be given a gown to wear during the test.
You may lie on your left side with your knees pulled up to your belly. Because you will be given medicine during the colonoscopy, you probably won’t remember much, if anything, until you wake up after the procedure.
Next, the doctor will insert a thin, flexible colonoscope in your anus and move it slowly through the rectum and into your colon. Air will be used to inflate your colon so the doctor can look at the lining of the colon through the scope or on a computer screen hooked to the scope.
During the test
You may feel the need to have a bowel movement while the scope is in your colon. You may also feel some cramping. Breathe deeply and slowly through your mouth to relax your belly muscles. This should help the cramping. You will likely feel and hear some air escape around the scope. There is no need to be embarrassed about it. The passing of air is expected. You may be asked to change your position during the test.
Your doctor will look at the whole length of your colon as the scope is gently moved in and then out of your colon.
The doctor may also use tiny tools, such as forceps, loops, or swabs, through the scope to collect tissue samples (biopsy) or take out growths. Usually, people do not feel anything if a biopsy is done or if polyps are taken out.
The scope is slowly pulled out of your anus and the air escapes. Your anal area will be cleaned with tissues. If you are having cramps, passing gas may help relieve them.
The test usually takes 30 to 45 minutes, but it may take longer, depending upon what is found and what is done during the test.
After the test
After the test, you may need to stay at the clinic for 1 to 2 hours. Or you may be allowed to leave sooner with the person who will be driving you home. Your doctor will tell you when you can eat your normal diet and do your normal activities. Drink a lot of fluid after the test to replace the fluids you may have lost during the colon prep, but do not drink alcohol.
If you received a sedative during the test, do not drive, operate machinery, or sign legal documents for 24 hours after the test. Arrange to have someone drive you home after the test.
How It Feels
The colon prep will cause diarrhea. Some people also have cramping.
During the test, you may feel very sleepy and relaxed from the sedative and pain medicines. You may have cramping or feel brief, sharp pain when the scope is moved or air is blown into your colon. As the scope is moved up the colon, you may feel the need to have a bowel movement and pass gas. If you are having pain, tell your doctor.
The suction machine used to remove stool (feces) and secretions may be noisy but does not cause pain.
You will feel sleepy after the test for a few hours. Many people say they do not remember very much about the test because of the sedative.
After the test, you may have bloating or crampy gas pains and may need to pass some gas. If a biopsy was done or a polyp taken out, you may have traces of blood in your stool (feces) for a few days. If polyps were taken out, your doctor may instruct you to not take aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) for 7 to 14 days.
Risks
There is a small chance for problems from a colonoscopy. The scope or a small tool may tear the lining of the colon or cause bleeding.
After the test
After the test, call your doctor immediately if you:
- Have heavy rectal bleeding.
- Have severe belly pain.
- Develop a fever.
- Are very dizzy.
- Are vomiting.
- Have a swollen and firm belly.
Problems such as heavy rectal bleeding may not occur until several weeks after a colonoscopy. This isn’t common. But it can happen after polyps are removed.
Results
Colonoscopy is a test that allows your doctor to look at the inner lining of your large intestine (rectum and colon). If a sample of tissue (biopsy) was collected during the colonoscopy, it will be sent to a lab for tests.
- Samples of colon tissue are usually sent to a pathology lab, where they are looked at under a microscope for diseases.
- Other samples of colon tissue may be sent to a microbiology lab to see whether an infection is present.
Your doctor may be able to tell you the results immediately after the procedure. Other test results are ready in 2 to 4 days. Test results for certain infections may be ready in several weeks.
|
Normal: |
The lining of the colon looks smooth and pink, with a lot of normal folds. No growths, pouches, bleeding, or inflammation are present. |
|
Abnormal: |
Some abnormal findings of colonoscopy include hemorrhoids (the most common cause of blood in the stool), polyps, cancer, one or more sores ( ulcers), pouches in the wall of the colon ( diverticulosis), or inflammation. A red, swollen lining of the colon (colitis) may be caused by infection or inflammatory bowel disease (IBD). |
What Affects the Test
Reasons you may not be able to have the test or why the results may not be helpful include:
- Having a barium enema within a week before the test. Barium can block your doctor’s view of the colon.
- Not doing a good colon prep before the test. If you still have stool (feces) in the colon, your doctor may cancel the test and you will have to reschedule and do the colon prep again.
- Having a colon that has many turns, past surgery on the colon, or a lot of pain during the test.
- Taking iron supplements. This may make your stool turn black and make it hard to clean out the colon. Do not take iron supplements for several days before a colonoscopy.
- Drinking red or purple fluids, such as grape juice or fruit punch.
- Eating red or purple foods, such as grape ice pops or cherry gelatin.
What To Think About
- In general, pregnant women and people who have an abdominal infection or an attack of diverticulitis should not have a colonoscopy unless there is an important reason for it.
- Colonoscopy is a more expensive procedure than a stool test or other endoscopic colon test (such as sigmoidoscopy), but it can be done less often over time if results are normal.
- Your doctor may recommend earlier or more frequent testing if you have a higher risk for colorectal cancer. Talk to your doctor about when you should be tested.
References
Other Works Consulted
- Chernecky CC, Berger BJ (2013). Laboratory Tests and Diagnostic Procedures, 6th ed. St. Louis: Saunders.
- Fischbach FT, Dunning MB III, eds. (2009). Manual of Laboratory and Diagnostic Tests, 8th ed. Philadelphia: Lippincott Williams and Wilkins.
- Levin B, et al. (2008). Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: A joint guideline from the American Cancer Society, the U.S. Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. CA: A Cancer Journal for Clinicians, 58(3): 130–160.
- Pagana KD, Pagana TJ (2010). Mosby’s Manual of Diagnostic and Laboratory Tests, 4th ed. St. Louis: Mosby Elsevier.
- U.S. Preventive Services Task Force (2008). Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Available online: http://www.uspreventiveservicestaskforce.org/uspstf/uspscolo.htm.
Current as of: December 19, 2018
Author: Healthwise Staff
Medical Review:Adam Husney MD – Family Medicine & E. Gregory Thompson MD – Internal Medicine & Kathleen Romito MD – Family Medicine & Arvydas D. Vanagunas MD – Gastroenterology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.