Total Hip Replacement Surgery
Surgery Overview
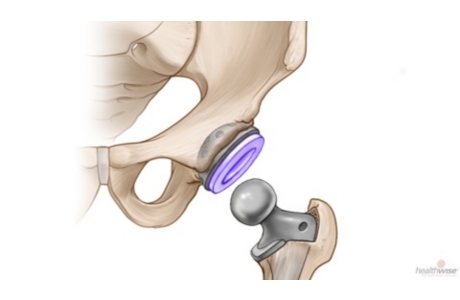
Total hip replacement is a step-by-step surgery to replace the ball at the top of the thighbone (femur) and the hip socket.
Doctors use metal, ceramic, or plastic replacement parts. They may be attached to the bones in one of two ways:
- Cemented to the bone.
- Uncemented. These parts have a porous coating that the bone grows into.
Your doctor may use general anesthesia. This means you’ll be asleep during surgery. Or a doctor may use regional anesthesia. This means you can’t feel the area of the surgery. You’ll have medicine that makes you unaware but lightly asleep. Which type of anesthesia you get depends on your doctor and your overall health. Your doctor might also ask what you prefer.
Types of surgery
In traditional hip replacement surgery, the doctor makes a 6- to 10-inch cut (incision) on the side or the back of your hip. Some muscles and other soft tissues, such as ligaments, are cut so the doctor can get to the hip joint.
Hip replacement can also be done with one or two smaller incisions. This is called minimally invasive surgery. It may cause less blood loss and leave a smaller scar. But it can also mean a longer time in surgery, because the surgery is harder to do. And if the new hip can’t be fitted properly through the smaller incision, the doctor may have to make a larger cut.
A newer type of surgery is done through a small incision in the front (anterior) of the hip. Anterior hip surgery causes less damage to muscles and other soft tissues than getting to the hip joint from the side or the back. It may help you heal faster and return to activity sooner.
Anterior surgery and minimally invasive surgery require special training and equipment. Your doctor can explain your options and help you understand the risks and benefits of each type of surgery.
What To Expect
Right after surgery
Your pain will be controlled with intravenous (IV) medicine. You will probably also have medicines to prevent infection, blood clots, and nausea. If you had regional anesthesia, you may have little or no feeling below your waist for a while.
You may have a cushion between your legs. It helps keep your new hip in the correct position. You may also have a catheter. It lets you empty your bladder without getting up. To help prevent blood clots, you may be wearing compression stockings. And you may have compression sleeves on your legs. These squeeze and release your lower legs to help keep the blood moving.
Moving around
On the day of surgery or the day after, you’ll get out of bed with help. You will learn how to walk with a walker or crutches. By the time you leave the hospital, you will be able to safely sit down and stand up, dress yourself, use the toilet, bathe, and use stairs.
As soon as possible, you will start physical therapy. You’ll learn exercises to help you get stronger. You will also be taught how to move your body without dislocating your hip.
If you have traditional surgery, you will need to follow “hip precautions” until your hip is fully healed. Most often, this means that you:
- Avoid twisting at the hips. You keep your shoulders, hips, knees, and feet facing forward.
- Do not bend your hip more than 90 degrees. This means no bending forward while sitting down and no bending over to tie your shoes.
- Do not let your affected leg cross the center of your body toward the other leg. Your therapist may suggest that you:
- Do not cross your legs or feet.
- Be very careful as you get in or out of bed or a car. Make sure your leg does not cross that imaginary line down the middle of your body.
- Keep a pillow between your knees when you are lying down.
There is a much lower risk of hip dislocation after anterior surgery, so there are fewer precautions. Your physical therapist will teach you how to move safely. For example, while you’re healing, the therapist may suggest that you:
- Do not step backwards or bend backwards.
- Do not turn your leg too far out to the side. Keep your toes pointing forward or slightly in.
Leaving the hospital
Your doctor will let you know if you will stay in the hospital or if you can go home the day of surgery. When you go home, you will need someone to help you for the next few weeks or until you have more energy and can move around better. Some people who need more extensive rehab may go to a specialized rehab center for more treatment.
Continued recovery
During the first week or so after surgery, you will need less and less pain medicine. For a few weeks after surgery, you will probably take medicine to prevent blood clots.
You may need a walker, crutches, or a cane for a few weeks. As you get your energy back, work up to taking a short walk a few times each day. If you feel any soreness, try a cold pack on your hip.
Don’t drive until:
- Your doctor says it is okay for you to drive.
- You have stopped taking an opioid pain medicine.
After traditional surgery, complete recovery can take at least 6 months. Recovery is usually faster after anterior hip surgery. Keep up your walking and physical therapy exercises. They help speed your recovery.
For most people, it is safe to have sex about 4 to 6 weeks after a hip replacement. Talk to your doctor about when it is okay to have sex and what positions are safe for your hip. Some positions could cause you to dislocate your hip. That means that your doctor may want you to avoid certain positions, especially for the first few months.
Living with a hip replacement
Exercise (such as swimming and walking) is important for building your muscle strength. And it helps you feel better overall. Discuss with your doctor what type of exercise is best for you.
- You probably will be able to return to most activities that you did before surgery, such as golfing, biking, swimming, or dancing.
- Your doctor may want you to avoid running, playing tennis, and doing other things that put a lot of stress on the joint.
Your doctor will probably want to see you at least once a year to check your hip.
For at least 2 years after your surgery, your doctor may want you to take antibiotics before dental work or any invasive procedure. This is to help prevent infection around your hip implant. After 2 years, your doctor and dentist will decide if you still need to take antibiotics.
Why It Is Done
Total hip replacement surgery is usually done when hip pain and loss of function become severe and when treatment no longer relieves pain. Hip replacement is sometimes done after a hip fracture.
How Well It Works
Surgery usually works well. You will probably have much less pain and be able to do most of your daily activities more easily. But recovery does take time and patience.
Most artificial hip joints will last for 10 to 20 years or longer. It depends on your age, how much stress you put on the joint, and how well your new joint and bones mend. Your weight can make a difference. Every extra pound of body weight adds 3 pounds of stress to your new hip joint. Controlling your weight will help your new hip joint last longer.
Risks
The risks of hip replacement surgery can be divided into two groups:
- Risks of the surgery and recovery period. These risks include:
- Blood clots. These can be dangerous if they block blood flow from the leg back to the heart, or if they move to the lungs.
- Infection. Infection in the wound is usually treated with antibiotics. Infection deep in the joint may need more surgery. In some cases, the hip implant has to be replaced with another one.
- Nerve injury. This is rare. It can cause tingling, numbness, or difficulty moving a muscle.
- Problems with wound healing.
- Problems with anesthesia.
- Hip dislocation after surgery.
- Difference in leg length. Any difference is usually very small and can be corrected by using a shoe insert.
- Long-term risks that may occur months to years after the surgery. These risks include:
- Loosening of the hip implant in the bone.
- Infection in the joint.
- A reaction to the metal in the new hip joint. As metal ball and socket parts rub against each other, tiny bits of the surface of the parts wear off. Some people are sensitive to the types of metal that may be used for joint replacement.
What To Think About
You may donate your own blood to use during surgery if needed. This is called autologous blood donation. If you choose to do this, start the donation several weeks before the surgery so that you have time to donate enough blood and rebuild your blood volume before surgery.
If you need more than one joint replacement surgery, such as a knee and a hip, talk to your doctor. There are guidelines that may help you and your doctor decide which surgery to do first.
References
Other Works Consulted
- Imamura M, et al. (2012). Single mini-incision total hip replacement for the management of arthritic disease of the hip: A systematic review and meta-analysis of randomized controlled trials. Journal of Bone and Joint Surgery, American Version, 94(20): 1897–1905.
- Rethman MP, et al. (2012). Prevention of Orthopaedic Implant Infection in Patients Undergoing Dental Procedures: Executive Summary on the AAOS/ADA Clinical Practice Guideline. Available online: http://www.aaos.org/research/guidelines/PUDP/dental_guideline.asp.
Credits
Current as of: June 26, 2019
Author: Healthwise Staff
Medical Review:Kathleen Romito MD – Family Medicine & Adam Husney MD – Family Medicine & E. Gregory Thompson MD – Internal Medicine & Jeffrey N. Katz MD, MPH – Rheumatology
Current as of: June 26, 2019
Author: Healthwise Staff
Medical Review:Kathleen Romito MD – Family Medicine & Adam Husney MD – Family Medicine & E. Gregory Thompson MD – Internal Medicine & Jeffrey N. Katz MD, MPH – Rheumatology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.