Urinary Tract Infections in Teens and Adults
Topic Overview
Is this topic for you?
This topic is about urinary tract infections in teens and adults. For information about infections in babies and young children, see the topic Urinary Tract Infections in Children.
What is a urinary tract infection?
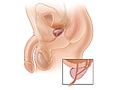
Your urinary tract is the system that makes urine and carries it out of your body. It includes your bladder and kidneys and the tubes that connect them. When germs get into this system, they can cause an infection.
Most urinary tract infections (UTIs) are bladder infections. A bladder infection usually is not serious if it is treated right away. If you do not take care of a bladder infection, it can spread to your kidneys. A kidney infection is serious and can cause permanent damage.
What causes urinary tract infections?
Usually, germs get into your system through your urethra, the tube that carries urine from your bladder to the outside of your body. The germs that usually cause these infections live in your large intestine and are found in your stool. If these germs get inside your urethra, they can travel up into your bladder and kidneys and cause an infection.
Women tend to get more bladder infections than men. This is probably because women have shorter urethras, so it is easier for the germs to move up to their bladders. Having sex can make it easier for germs to get into a woman’s urethra.
You may be more likely to get an infection if you have diabetes or you are pregnant. The chance that you will get a bladder infection is higher if you have any problem that blocks the flow of urine from your bladder. Examples include having kidney stones or an enlarged prostate gland.
For reasons that are not well understood, some women get bladder infections again and again.
What are the symptoms?
You may have an infection if you have any of these symptoms:
- You feel pain or burning when you urinate.
- You feel like you have to urinate often, but not much urine comes out when you do.
- You have pain in your lower belly.
- Your urine is cloudy, looks pink or red, or smells bad.
- You have pain on one side of your back under your ribs. This is where your kidneys are.
- You have fever and chills.
- You have nausea and vomiting.
Call your doctor right away if you think you have an infection and:
- You have a fever, nausea and vomiting, or pain in one side of your back under your ribs.
- You have diabetes, kidney problems, or a weak immune system.
- You are older than 65.
- You are pregnant.
How are urinary tract infections diagnosed?
Your doctor will ask for a sample of your urine. It is tested to see if it has germs that cause bladder infections.
If you have infections often, you may need extra testing to find out why.
How are they treated?
Antibiotics prescribed by your doctor will usually cure a bladder infection. It may help to drink lots of water and other fluids and to urinate often, emptying your bladder each time.
For urinary symptoms such as pain or burning, there is a medicine you can buy without a prescription. Phenazopyridine (such as Azo-Gesic, Azo-Standard, and Uristat) can relieve these symptoms. But phenazopyridine doesn’t treat the infection, so you’ll still need an antibiotic.
If your doctor prescribes antibiotics, take the pills exactly as you are told. Do not stop taking them just because you feel better. You need to finish taking them all so that you do not get sick again.
Can urinary tract infections be prevented?
You may be able to help prevent these infections.
- Take time to empty your bladder as much as possible when you urinate.
- If you are a sexually active woman, make it a point to urinate shortly after having sex.
- If you are a woman past menopause who is having repeated UTIs, using vaginal estrogen may help.
Cause
Bacteria that enter the urethra and travel up the urinary tract are the usual cause of urinary tract infections (UTIs). Bacteria that normally live in the large intestine and are present in feces (stool) are the most common source of infection. Sexual intercourse may move bacteria into the urinary tract, especially in women. Catheters, which are small, flexible tubes inserted into the bladder to allow urine to drain, are a common source of bacterial infection in people who are in hospitals or who live in long-term care facilities.
Sometimes bacteria traveling through the blood or lymph system cause kidney or bladder infections.
Kidney stones, an enlarged prostate in men, and structural problems in the urinary tract can contribute to UTIs by limiting the body’s ability to eliminate urine completely.
Women who have repeated UTIs may have inherited genes that make them more likely to get these infections.
Symptoms
Symptoms of a urinary tract infection (UTI) may include:
- Pain or burning when you urinate.
- An urge to urinate frequently but usually passing only small amounts of urine.
- Pain in the lower belly.
- Urine that looks cloudy, is pink or red, or smells bad.
- Pain in the flank, which is felt just below the rib cage and above the waist on one or both sides of the back.
- Fever and chills.
- Nausea and vomiting.
Some people have bacteria in their urinary tract without having any symptoms. This is called asymptomatic bacteriuria. Asymptomatic bacteriuria may lead to infections that cause symptoms, but in many cases it does not. It usually goes away without treatment.
Several other conditions, such as vaginal infections or irritable bladder, cause symptoms similar to those of a UTI. Your doctor may evaluate your health for one or more of these if you have urinary symptoms, depending on your medical history and how well you respond to treatment for a UTI.
What Happens
Urinary tract infections (UTIs) typically occur when bacteria from the rectal area enter through the urethra and travel up the urinary tract to the bladder or kidneys.
Typically, UTIs cause urinary symptoms, such as pain or burning during urination. Some mild bladder infections may go away on their own within a couple of days. Most UTIs clear up quickly with antibiotics. The amount of time required to cure the infection and the need for urine tests will vary with the location (bladder or kidneys), frequency, and seriousness of the infection. Kidney infections and UTIs that are complicated by other factors require longer treatment.
Complications of UTIs are not common but do occur. Serious complications can include permanent kidney damage and widespread infection (sepsis), which can be life-threatening. The risk is greater if the infection is not treated or if the infection does not respond to antibiotics.
Some people have many UTIs. They are often new infections (recurrent UTIs), but they can also be the same infection coming back (a relapse). A rapid relapse usually means that treatment failed or there is another problem affecting the urinary tract (not just the infection).
UTIs in women
UTIs are most common in young to middle-aged women. They occur more often in women than in men because:
- The rectum is closer to the urine outlet (urethra) in women than in men. This allows bacteria present in stool to enter the urinary tract more easily.
- The urethra is shorter in women than in men, which allows bacteria to reach the bladder more easily.
- In women, sexual intercourse can push bacteria into the urethra.
- The fluid produced by a man’s prostate gland helps kill bacteria in his urinary tract.
Some women have an ongoing problem with UTIs. If a woman has more than two bladder infections in 6 months or more than three infections in a year, she is said to have recurrent UTIs. Recurrent UTIs usually get better with extended antibiotic treatment. But infection may recur as soon as the woman stops taking antibiotics. For this reason, doctors usually recommend preventive antibiotics.
UTIs in men
Most urinary tract infections in men are caused by bacteria.
UTIs in older men are more often related to prostate problems. This can make them more difficult to treat. Having an enlarged prostate, which is common in older men, can limit the body’s ability to pass urine. Repeated UTIs may indicate prostatitis, epididymitis, or another urinary tract problem.
For more information, see:
What Increases Your Risk
Risk factors in women
Urinary tract infections (UTIs) are most common in young to middle-aged sexually active women. Things that increase a woman’s risk of getting UTIs include:
- Sexual activity, which pushes bacteria into the urethra. Sexual activity with the use of a diaphragm and spermicide raises the risk.
- Pregnancy.
- Previous UTIs.
- Lack of estrogen, which allows bacteria that can cause UTIs to grow more easily in the vagina or urethra. Women who have gone through menopause are at increased risk for UTIs.
Risk factors in men
Things that increase a man’s risk of UTIs include:
- Problems with the prostate gland. Men become increasingly prone to UTIs as they get older because of prostate problems, such as enlarged prostate (benign prostatic hyperplasia) and prostatitis.
- An uncircumcised penis.
- Anal intercourse.
- Unprotected sex with a woman who has a vaginal infection.
- HIV infection.
Risk factors in both women and men
Certain risk factors apply to both women and men. These include:
- Having a catheter in place. Bacteria can enter the catheter and start an infection. Most at risk are older adults who are in hospitals or who live in long-term care facilities.
- Kidney stones and other obstructions in the urinary tract. These may block the flow of urine, raising the risk of bacterial infection.
- Diabetes. People with diabetes are at greater risk for UTIs because their immune systems are weakened. Also, long-term high blood sugar can damage the kidneys’ filtering system (diabetic nephropathy).
- Structural problems of the urinary tract. These may be present at birth or develop later in life.
When should you call your doctor?
Call your doctor immediately if painful urination or other symptoms of a urinary tract infection (UTI) occur with:
- Nausea and vomiting.
- Fever and chills.
- Pain in the flank, which is felt just below the rib cage and above the waist on one or both sides of the back, or lower belly pain.
Call your doctor immediately if you are pregnant and have symptoms of a UTI (listed above).
Call a doctor if you:
- Have had UTI symptoms previously and have those symptoms again.
- Have minor symptoms of a UTI that do not clear up in 1 to 2 days, such as pain or burning when you urinate, foul-smelling urine, or the urge to urinate frequently while passing only small amounts of urine.
- Notice blood or pus in your urine.
- Have symptoms of a UTI and you have diabetes.
- Have been taking antibiotics for a UTI but your symptoms do not improve or they come back (recur) after improving temporarily.
Watchful waiting
Watchful waiting is a wait-and-see approach. If you get better on your own, you won’t need treatment. If you get worse, you and your doctor will decide what to do next.
In adults, home treatment for minor urinary tract infections (UTIs) often resolves the problem. Home treatment includes drinking plenty of water and urinating often, emptying the bladder each time.
- Try home treatment for 1 to 2 days if your symptoms are minor.
- If your symptoms last longer than 1 to 2 days or are severe, seek medical help.
Watchful waiting is not appropriate if you:
- Have diabetes or an impaired immune system.
- Are pregnant.
- Are older than 65.
Who to see
The following health professionals can treat urinary tract infections (UTIs):
Exams and Tests
If you have symptoms of a urinary tract infection (UTI), your first evaluation by a doctor will likely include:
- A medical history and physical exam.
- Urinalysis.
Your doctor may order a urine culture to confirm the diagnosis of a suspected UTI. But if your doctor thinks you have a UTI, he or she may have you start taking antibiotics right away without waiting for the results of your test.
Tests used less frequently
If the infection does not respond to treatment with antibiotics or recurs rapidly, if the infection may be complicated by other factors, or, in some cases, if the kidneys are infected, your doctor may order other tests to:
- Look for the cause of recurrent or chronic infections.
- Check for other kidney problems.
- Diagnose structural problems of the urinary tract that might make you more likely to get UTIs.
- Find out whether the infection is caused by unusual bacteria.
- Find out whether you have an impaired immune system.
If you get UTIs often, your doctor may write you a standing prescription for antibiotics that you can fill without a doctor’s appointment. Then when you first have symptoms of a UTI, you can start taking medicine right away. You may want to use a home test for UTI to make sure you have an infection before you start antibiotics.
Treatment Overview
Antibiotics can treat most urinary tract infections (UTIs) successfully. The goals of treatment for UTIs are to relieve symptoms, eliminate the infection and prevent recurrence, and prevent unlikely but serious complications such as kidney damage and sepsis. In pregnant women, treatment protects the woman and the fetus.
Initial treatment
Treatment for bladder infections is usually a combination of antibiotics and home treatment. Home treatment includes drinking a lot of water and fluids and urinating frequently, emptying your bladder each time. More testing is not needed if your symptoms improve.
Oral antibiotics usually can treat kidney infections (pyelonephritis). But you may need a brief hospital stay and a short course of intravenous (IV) antibiotics if you are too ill or nauseated to take medicine by mouth (oral medicine). Kidney infections tend to make people more severely ill than bladder infections.
You may need more tests before and after treatment if you:
- Are pregnant.
- Are older than 65.
- Have diabetes or an impaired immune system.
- Are a man.
If you have a severe kidney infection, or if a bladder or kidney infection is complicated by other factors, you may need hospital care.
Treatment if the condition gets worse or recurs
If your urinary tract infection (UTI) does not improve after treatment with antibiotics, you will need further evaluation and additional antibiotic treatment.
If the infection spreads and affects your kidney function or causes widespread infection (sepsis), you will need hospital care. These complications are not common. And they rarely occur in people who are otherwise healthy.
A new infection, rather than a relapse of the same infection, usually is the cause of a UTI that keeps coming back (recurs).
- Women with recurrent bladder infections may be treated with preventive antibiotic therapy.
- Recurrent UTIs in men are usually a sign of prostate infection (prostatitis). Chronic prostatitis can be hard to treat. For more information, see the topic Prostatitis. Follow-up checkups are usually needed for men who have UTIs and are always needed if the infection recurs.
Prevention
You can take steps to prevent new or relapsing urinary tract infections (UTIs).
Prevention tips for men and women
- Drinking more water and other liquids may help.
- When you urinate, take time to empty your bladder as much as possible.
Prevention tips for women
- Urinate immediately after sexual intercourse. This is the best protection women have against UTIs, because it helps prevent bacteria from moving into the urethra.
- Avoid using condoms coated with spermicide or a diaphragm for birth control if your doctor believes they are causing you to get UTIs.
- Change sanitary napkins often.
- Wipe from front to back after using the toilet to avoid spreading bacteria from your anus to your urinary tract.
- Some women have found cranberry juice to be helpful, although the evidence from studies isn’t strong.
- If you get UTIs often, ask your doctor about taking antibiotics right after sexual intercourse to prevent recurrent UTIs.
- Post-menopausal women may want to ask their doctors about using vaginal estrogen to prevent recurrent UTIs.
Prevention tip for men
Keep the tip of your penis clean, especially if you are uncircumcised. The foreskin can trap bacteria, which can then get into the urinary tract and cause infection.
Home Treatment
Some people who have had a UTI in the past may be able to avoid getting another infection by taking action at the first sign of any pain or burning with urination. Here are some tips:
- Drink lots of water, especially during the first 24 hours after your symptoms appear. This will help make the urine less concentrated and wash out the infection-causing bacteria. This may alter some of your body’s normal defense mechanisms. But most doctors recommend drinking a lot of fluids when you have a UTI.
- Urinate frequently and completely, to empty your bladder each time.
But these steps won’t cure a UTI, so don’t delay getting medical treatment and starting on an antibiotic if you have an infection.
To relieve pain, take a hot bath or lay a heating pad over your genital area. Never go to sleep with a heating pad in place.
Self-treatment of recurrent UTIs
If you are a woman who has frequent uncomplicated UTIs, your doctor may write a standing prescription for antibiotics to take if you notice symptoms of a UTI. If you and your doctor agree to follow this approach and you start to have symptoms that you are certain are caused by a UTI, follow your doctor’s instructions for taking the medicine and for watching your symptoms. Be sure to tell your doctor if your symptoms do not improve or if you start having UTIs more often than in the past.
Medications
Oral antibiotics can treat most bladder infections and uncomplicated kidney infections successfully. In many cases, if the symptoms and urinalysis suggest a urinary tract infection (UTI), you will start taking antibiotics without waiting for the results of a urine culture.
The number of days your doctor will have you take antibiotics depends on your infection and the type of antibiotic medicine.
Antibiotics for recurrent infections
Doctors sometimes advise that women with repeat infections use preventive antibiotic therapy. This may include taking a small dose of antibiotics daily or on alternate days, taking antibiotics after sexual intercourse (since sex often triggers UTIs in women with recurrent infections), or taking antibiotics only when you develop symptoms. Talk with your doctor about which treatment strategy is right for you.
Medication choices
Medicines used to treat UTIs include:
- Antibiotics to cure the infection. Antibiotics used for UTIs include sulfonamides with trimethoprim (such as Bactrim).
- Phenazopyridine (such as Uristat) to treat the pain and burning of a UTI. Uristat is an example of phenazopyridine you can buy without a prescription.
- Other nonprescription medicines for pain. These include acetaminophen (such as Tylenol) and nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (for example, Advil) and naproxen (for example, Aleve).
Medicines used to prevent recurrent UTIs include:
- Antibiotics, including sulfonamides with trimethoprim (such as Bactrim).
- Methenamine (such as Hiprex).
- Vaginal estrogen (such as Estrace, Estring, or Vagifem) for women who have been through menopause.
Be safe with medicines. Read and follow all instructions on the label. Be sure to tell your doctor if you are or think you may be pregnant. Some of these medicines are not safe to use if you are pregnant.
What to think about
These medicines are often prescribed in a less costly generic form rather than under a brand name. A pharmacist might also decide to give you a generic instead of a brand name medicine unless the prescription says “no generic.”
Take all of the antibiotics your doctor has prescribed. Most people begin to feel better soon after they begin the medicine. But if you stop taking the medicine as soon as you feel better, the infection may return. And not taking the full course of antibiotics encourages the development of bacteria that are resistant to antibiotics. This not only makes antibiotics less effective but also makes bacterial infections harder to treat.
Current as of: December 19, 2018
Author: Healthwise Staff
Medical Review:E. Gregory Thompson, MD – Internal Medicine & Adam Husney, MD – Family Medicine & Elizabeth T. Russo, MD – Internal Medicine & Avery L. Seifert, MD, FACS – Urology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.