Decompressive Laminectomy for Lumbar Spinal Stenosis
Surgery Overview
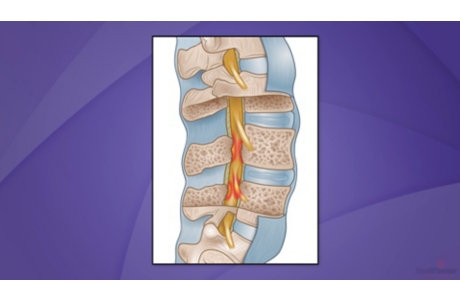
Decompressive laminectomy is the most common type of surgery done to treat lumbar (low back) spinal stenosis. This surgery is done to relieve pressure on the spinal nerve roots caused by age-related changes in the spine. It also is done to treat other conditions, such as injuries to the spine, herniated discs, or tumors. In many cases, reducing pressure on the nerve roots can relieve pain and allow you to resume normal daily activities.
Laminectomy removes bone (parts of the vertebrae) and/or thickened tissue that is narrowing the spinal canal and squeezing the spinal nerve roots. This procedure is done by surgically cutting into the back.
Spinal fusion
In some cases, spinal fusion (arthrodesis) may be done at the same time to help stabilize sections of the spine treated with decompressive laminectomy. Spinal fusion is major surgery, usually lasting several hours. There are different methods of spinal fusion:
- In the most common method, bone is taken from elsewhere in your body or obtained from a bone bank. This bone is used to make a “bridge” between adjacent spinal bones (vertebrae). This “living” bone graft stimulates the growth of new bone.
- In some cases an additional fusion method (called instrumented fusion) is done in which metal implants (such as rods, hooks, wires, plates, or screws) are secured to the vertebrae to hold them together until new bone grows between them.
There are a variety of specialized techniques that can be used in spinal fusion, although the basic procedure is the same. Techniques vary from what type of bone or metal implants are used to whether the surgery is done from the front (anterior) or back (posterior) of the body. The method chosen depends on a number of things, including your age and health condition, how many vertebrae are involved, the severity of nerve root pressure and associated symptoms, and the surgeon’s experience. Spinal fusion increases the possibility of complications and the recovery time after surgery.
What To Expect
Depending on your health and the extent of the surgery, it may take several months or more before you are able to return to your normal daily activities.
Why It Is Done
Surgery for spinal stenosis is considered when:
- Severe symptoms restrict normal daily activities and become more severe than you can manage.
- Nonsurgical treatment does not relieve pain, and severe nerve compression symptoms of spinal stenosis (such as numbness or weakness) are getting worse.
- You are less able to control your bladder or bowels than usual.
- You notice sudden changes in your ability to walk in a steady way, or your movement becomes clumsy.
The decision to have surgery is not based on imaging test results alone. Even if the results of imaging tests show increased pressure on the spinal cord and spinal nerve roots, the decision to have surgery also depends on the severity of symptoms and your ability to do normal daily activities.
In some cases, spinal fusion will be done at the same time to stabilize the spine. Spinal fusion might make it easier for you to move around (improve function) and relieve your pain. It can also help keep the bones from moving into positions that squeeze the spinal canal and put pressure on the spinal nerve roots.
How Well It Works
Surgery for spinal stenosis usually is elective but may be recommended if symptoms cannot be relieved with nonsurgical treatment. In general, experts feel that surgery has good results and relieves pain in the lower extremities for people who have severe symptoms of spinal stenosis and who have few other serious health problems.
Research shows that:
- Surgery may work better than nonsurgical treatments to relieve pain and help you move better. If nonsurgical treatments have not worked well enough, surgery might be able to help you.footnote 1
- By 3 months, people who had surgery notice more improvement in their symptoms and can be more active than people who did not have surgery.footnote 1 This difference continues for at least 4 years after surgery.footnote 2
- The benefits of surgery appear to last for many years. After 8 to 10 years:
- People treated with surgery were as satisfied as those treated without surgery.
- People who had surgery were generally able to be more active and had less leg pain than those who had nonsurgical treatment.footnote 3
- Surgery appears to be more effective for leg pain than for back pain, but it may help both.footnote 4
But symptoms may return after several years. A second surgery may be needed if:
- Spinal stenosis develops in another area of the spine.
- An earlier surgical procedure was not effective in controlling symptoms.
- Instability develops, or fusion does not occur.
- Regrowth of tissue (lamina) presses on the spinal cord or spinal nerve roots.
Spinal fusion may be done at the same time as decompressive laminectomy. Spinal fusion may help to stabilize sections of the spine that have been treated with decompressive laminectomy. In general, fusion is only done if an area of the spine is unstable, which means the bones of the spine (vertebrae) move too much or do not move in a normal way. This extra movement causes wear and tear on the nerves or other soft tissues, leading to irritation and pain. The goal of fusion is to keep the damaged bones in the spine from moving so that the soft tissues are protected.
Risks
Complications from spinal stenosis surgery may result from the impact of other existing medical problems and the severity of the spinal problem. Also, all surgery poses risks of complications. These complications may be more serious in an older adult.
Possible complications include:
- Problems from anesthesia.
- A deep infection in the surgical wound.
- A skin infection.
- Blood clots.
- An unstable spine.
- Nerve injury, including weakness, numbness, or paralysis.
- Tears in the fibrous tissue that covers the spinal cord and the nerve near the spinal cord, sometimes requiring a second surgery.
- Trouble passing urine, or loss of bladder or bowel control.
- Long-term (chronic) pain, which develops after surgery in some cases.
- Death from problems caused by surgery, but this is rare.
If you have diabetes or circulation problems or if you are a smoker, you may be at greater risk for complications.
What To Think About
Most experts recommend that people with spinal stenosis try nonsurgical treatments before choosing surgery.
Surgery for lumbar spinal stenosis is most likely to relieve pain, numbness, and weakness that are mostly in your legs. Surgery may not work as well for relieving pain that is mostly in your back.
Surgery is usually effective if you have severe leg pain and numbness and you have not been able to move around well for a long time. But in some cases, the symptoms return after surgery. It is also possible that nerve symptoms, including numbness and clumsiness, may not be relieved or may return.
After a laminectomy and fusion, spinal stenosis may develop directly above or below the surgery site. Repeated surgeries for spinal stenosis increase your risk of complications and instability in the spine.
Age should not be a factor in deciding whether to have decompressive laminectomy. But if you have other medical conditions that will make this procedure and follow-up rehabilitation less successful, surgery may not be recommended.
References
Citations
- Weinstein JN, et al. (2008). Surgical versus nonsurgical therapy for lumbar spinal stenosis. New England Journal of Medicine, 358(8): 794–810.
- Weinstein JN, et al. (2010). Surgical versus nonoperative treatment for lumbar spinal stenosis four-year results of the Spine Patient Outcomes Research Trial. Spine, 35(14): 1329–1338.
- Atlas SJ, et al. (2005). Long-term outcomes of surgical and nonsurgical management of lumbar spinal stenosis: 8- to 10-year results from the Maine Lumbar Spine Study. Spine, 30(8): 936–943.
- Pearson A, et al. (2011). Predominant leg pain is associated with better surgical outcomes in degenerative spondylolistheses and spinal stenosis: Results from the Spine Patient Outcomes Research Trial (SPORT). Spine, 36(3): 219–229.
Credits
Current as of: June 26, 2019
Author: Healthwise Staff
Medical Review:William H. Blahd, Jr., MD, FACEP – Emergency Medicine & Adam Husney, MD – Family Medicine & Kathleen Romito, MD – Family Medicine & Kenneth J. Koval, MD – Orthopedic Surgery, Orthopedic Trauma
Current as of: June 26, 2019
Author: Healthwise Staff
Medical Review:William H. Blahd, Jr., MD, FACEP – Emergency Medicine & Adam Husney, MD – Family Medicine & Kathleen Romito, MD – Family Medicine & Kenneth J. Koval, MD – Orthopedic Surgery, Orthopedic Trauma
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.