The journey to start a family can be filled with joy and anticipation, but for some couples, challenges arise when they try to conceive. In vitro fertilization (IVF) is a medical procedure that has brought hope to many such families, helping them overcome infertility issues and realize the dream of having a child. IVF testing plays a significant role in identifying potential genetic, hormonal, or other factors that may affect a couple’s ability to conceive or carry a healthy pregnancy to full term. These tests provide invaluable information for both patients and healthcare providers, helping to optimize treatment plans and increase the chances of success. In this article, we will delve into the world of IVF testing, discuss its various types, benefits, and limitations in a friendly, positive manner.
Types of IVF Testing
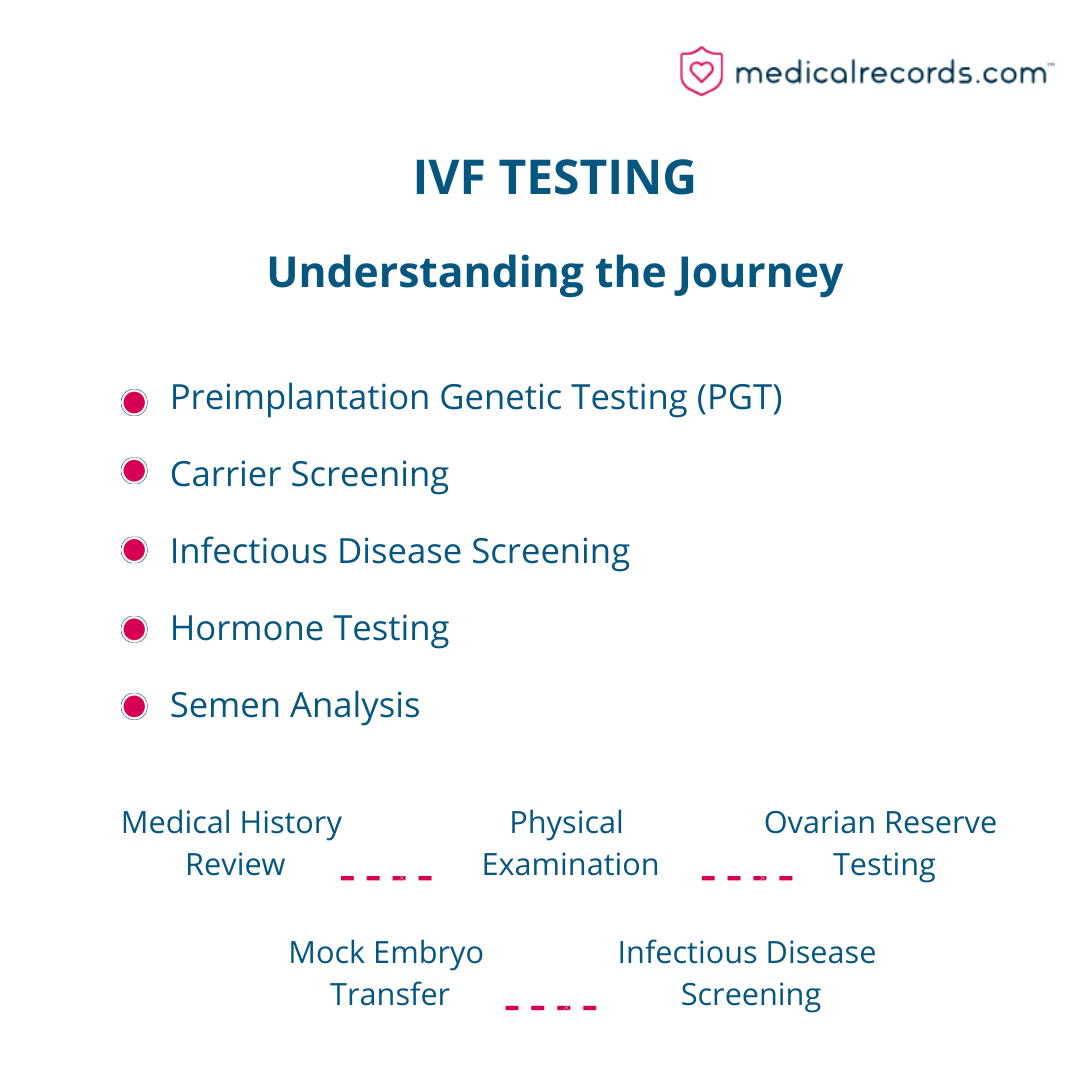
There are several types of IVF testing, each designed to assess specific aspects of a couple’s reproductive health. Knowing about these tests can empower couples and give them hope as they navigate their fertility journey.
- Preimplantation Genetic Testing (PGT): According to the American College of Obstetricians and Gynecologists (ACOG), Preimplantation Genetic Testing (PGT) testing analyzes the genetic makeup of embryos created through IVF to identify potential genetic disorders, chromosomal abnormalities, or other issues that could impact the success of a pregnancy. PGT allows couples to make informed decisions about their embryos, increasing their chances of having a healthy baby.
- Carrier Screening: genetic screening helps identify whether one or both partners are carriers of certain genetic diseases or disorders that could be passed on to their child. By knowing their carrier status, couples can make informed decisions about their family planning and minimize the risk of having a child with a genetic disorder.
- Infectious Disease Screening: As recommended by the Centers for Disease Control and Prevention (CDC), this screening checks for infections like HIV, hepatitis, and syphilis, which may impact the embryo’s health, uterus, or pregnancy. Detecting and treating these infections early can improve the chances of a successful pregnancy and a healthy baby.
- Hormone Testing: Hormone tests measure the levels of certain hormones in the body, which can help assess fertility and the likelihood of a successful pregnancy. Understanding their hormone levels can help couples address any imbalances and improve their overall reproductive health.
- Semen Analysis: This test evaluates sperm count, motility, and morphology to determine the quality of a man’s sperm, which is vital for fertilizing an egg. With this information, men can take steps to improve their sperm quality and increase their chances of becoming fathers.
Pre-IVF Counseling and Testing
Before beginning IVF treatment, couples typically undergo a series of pre-IVF counseling and testing sessions. These sessions provide a supportive environment for couples to learn about their reproductive health and address any potential issues that could affect their ability to conceive. The various steps in pre-IVF counseling and testing include:
- Medical history review: The healthcare provider will review both partners’ medical histories to identify potential factors that could impact fertility or pregnancy, such as a history of miscarriages, being overweight, smoking, or experiencing high levels of stress. Understanding their medical history can help couples make positive lifestyle changes to improve their fertility.
- Physical exam: Both partners will undergo a physical examination to assess their overall health and identify any potential issues that could affect their ability to conceive, such as polycystic ovary syndrome (PCOS) in women or varicocele in men. Early detection and treatment of these issues can increase the likelihood of a successful pregnancy.
- Ovarian reserve testing: This testing measures a woman’s egg supply and helps determine the likelihood of a successful pregnancy. According to the American Society for Reproductive Medicine (ASRM), a woman’s ovarian reserve declines with age, which can impact fertility. By understanding their ovarian reserve, women can make informed decisions about when to start a family and explore appropriate fertility treatments.
- Mock embryo transfer: This procedure simulates the embryo transfer process, helping to ensure that the actual transfer goes smoothly and increasing the chances of success. By practicing this crucial step, couples can feel more confident and prepared for their IVF journey.
- Infectious disease screening: Both partners will be screened for infections that could affect the health of the embryo, uterus, or pregnancy, as per CDC guidelines. Early detection and treatment of these infections can help protect the health of both the parents and the baby.
Preimplantation Genetic Testing (PGT)
PGT is a powerful tool in the IVF process, with three main types of testing that can provide couples with valuable insights into the health of their embryos:
- PGT-A (aneuploidy screening): ACOG states that this test analyzes embryos for chromosomal abnormalities that can lead to miscarriage or genetic disorders, such as Down syndrome. By identifying healthy embryos, couples can increase their chances of a successful pregnancy and a healthy child.
- PGT-M (monogenic/single gene disorder testing): This test identifies embryos with specific genetic disorders, such as cystic fibrosis or Tay-Sachs disease. By selecting embryos without these disorders, couples can minimize the risk of having a child with a genetic condition.
- PGT-SR (structural rearrangement testing): This test detects chromosomal rearrangements that can lead to miscarriage or congenital disabilities. By understanding the genetic health of their embryos, couples can make informed decisions about which embryos to transfer, increasing their chances of a successful pregnancy.
Carrier Screening
Carrier screening helps identify whether one or both partners are carriers of certain genetic disorders.
There are two main types of carrier screening that provide couples with valuable information about their genetic risk:
- Autosomal Recessive Carrier Screening: According to the National Institutes of Health (NIH), this screening identifies carriers of autosomal recessive disorders, such as cystic fibrosis or sickle cell anemia. By knowing their carrier status, couples can make informed decisions about their family planning and minimize the risk of having a child with a genetic disorder.
- X-Linked Carrier Screening: This screening identifies carriers of X-linked disorders, such as hemophilia or Duchenne muscular dystrophy. By understanding their carrier status, couples can make informed decisions about their family planning and work with their healthcare provider to manage any potential risks.
Hormone Testing
Hormone testing plays a vital role in assessing fertility and the likelihood of a successful pregnancy. Key hormones tested include:
- Follicle Stimulating Hormone (FSH): The ASRM states that this hormone stimulates the growth of eggs in the ovaries and is crucial for female fertility. By understanding their FSH levels, women can work with their healthcare provider to optimize their fertility.
- Luteinizing Hormone (LH): This hormone triggers ovulation and the release of an egg from the ovary, as per the ASRM. Monitoring LH levels can help couples time intercourse or fertility treatments to improve their chances of conception.
- Estradiol (E2): The ASRM also notes that this hormone helps regulate the menstrual cycle and is essential for the development of the uterine lining, which is necessary for a successful pregnancy. By monitoring E2 levels, couples can identify potential hormonal imbalances and address them to improve fertility.
Semen Analysis
Semen analysis is a critical component of male fertility assessment.
This test evaluates various aspects of a man’s sperm, including:
- Semen volume: According to the World Health Organization (WHO), this measures the amount of ejaculate produced during ejaculation, which can impact the likelihood of fertilizing an egg. Understanding semen volume can help men take steps to improve their reproductive health.
- Sperm count: The WHO also states that this evaluates the number of sperm present in the semen, with higher counts generally increasing the chances of fertilization. By knowing their sperm count, men can work with their healthcare provider to optimize their fertility.
- Sperm motility: This measures the ability of sperm to move, as sperm must be able to swim through the female reproductive tract to reach and fertilize an egg. Improving sperm motility can increase the chances of successful fertilization and conception.
- Sperm morphology: The ASRM mentions that this assesses the shape and structure of sperm, as abnormal sperm may have difficulty penetrating and fertilizing an egg. By addressing any issues with sperm morphology, men can improve their chances of becoming fathers.
Potential Risks and Limitations of IVF Testing
While IVF testing provides valuable information for optimizing treatment plans, it is essential to be aware of potential risks and limitations.
Being informed about these risks and limitations can help couples make educated decisions about their fertility journey:
- False positives/negatives: Some tests may produce false positive or negative results, which can lead to unnecessary worry or incorrect treatment decisions. By discussing these risks with their healthcare provider, couples can better understand the limitations of each test and make informed decisions about their treatment plan.
- Invasive procedures: Some IVF tests, like PGT, require invasive procedures that carry risks, such as infection or damage to the embryo. Couples should carefully weigh the benefits and risks of these tests with their healthcare provider to determine if they are appropriate for their situation.
- Emotional impact: IVF testing can be emotionally challenging, as couples may experience anxiety or disappointment if results are not what they hoped for. Seeking counseling and support can help couples navigate the emotional aspects of their fertility journey.
- Financial cost: IVF testing can be expensive, and not all tests are covered by insurance. Couples should discuss the costs and benefits of various tests with their healthcare provider to determine which tests are most appropriate for their situation.
Conclusion
IVF testing is an essential aspect of fertility treatment, helping to identify potential issues that may impact a couple’s ability to conceive or carry a healthy pregnancy. By undergoing various tests, couples can gain valuable insights into their reproductive health and work with their healthcare provider to develop a personalized treatment plan. It is important for couples to discuss their options with their healthcare provider, seek counseling and support, and carefully weigh the benefits and risks of each test to make informed decisions about their fertility journey. With the right information and support, many couples can overcome the challenges of infertility and achieve their dream of starting a family.
FAQ
What fertility tests are done before IVF?
Before starting the in vitro fertilization (IVF) process, doctors typically perform several fertility tests to evaluate the health and fertility of the prospective parents. These tests can include:
- Semen analysis: This test evaluates the sperm count, motility, and morphology of the male partner.
- Ovarian reserve testing: This involves measuring hormone levels, such as follicle-stimulating hormone (FSH) and anti-Müllerian hormone (AMH), to assess a woman’s egg supply and quality.
- Hormone testing: This includes testing for thyroid, prolactin, and other hormones that can impact fertility.
- Hysterosalpingogram (HSG): This X-ray procedure checks the fallopian tubes and uterus for any blockages or abnormalities.
- Transvaginal ultrasound: This imaging technique evaluates the uterus, ovaries, and surrounding pelvic structures for any abnormalities.
- Saline sonohysterogram (SIS): This test uses saline infusion and ultrasound to evaluate the uterus for polyps, fibroids, or other abnormalities.
- Laparoscopy or hysteroscopy: In some cases, doctors may recommend a minimally invasive surgical procedure to visualize and potentially treat any pelvic or uterine issues.
How long does PGS testing take IVF?
Preimplantation genetic screening (PGS) testing in IVF usually takes about one to two weeks.
The process involves:
- Embryo biopsy: A few cells are removed from the embryos on day five or six of their development.
- Genetic analysis: The biopsied cells are sent to a laboratory for genetic screening.
- Embryo selection: Based on the results, the doctor selects the most suitable embryos for transfer.
Can IVF test for autism?
Currently, there is no definitive test for autism during IVF. Autism is a complex neurological condition with multiple contributing genetic and environmental factors. While some specific genetic mutations have been associated with autism, the relationship between these genes and the development of the disorder is not yet fully understood.
Can you test for chromosomal abnormalities during IVF?
Yes, preimplantation genetic testing for aneuploidy (PGT-A) can be performed during IVF to screen embryos for chromosomal abnormalities. This testing helps identify embryos with the correct number of chromosomes, reducing the risk of miscarriage or chromosomal disorders such as Down syndrome, Edwards syndrome, or Patau syndrome.
Can you test for Down’s syndrome in IVF?
Yes, PGT-A testing during IVF can detect embryos with Down syndrome (trisomy 21) by identifying those that have an extra copy of chromosome 21. This can help reduce the risk of having a baby with Down syndrome.
How much is genetic testing for IVF?
The cost of genetic testing for IVF, such as PGT-A, varies depending on the clinic and the specific test being performed. On average, the cost ranges from $3,000 to $5,000. This is in addition to the standard IVF treatment costs.
How long does genetic testing take IVF?
Genetic testing during IVF, such as PGT-A, usually takes about one to two weeks from the time of embryo biopsy to receiving the results. This timeframe can vary depending on the specific test and laboratory being used.
How long after IVF can you take a pregnancy test?
After an IVF embryo transfer, it is generally recommended to wait at least nine to 12 days before taking a blood pregnancy test, known as a beta hCG test. This allows time for the hormone human chorionic gonadotropin (hCG) to reach detectable levels in the blood. Home urine pregnancy tests should be taken after 14 days to ensure accuracy, as they may not detect hCG as early as a blood test.
What is a beta test IVF?
A beta test, also known as a beta hCG test, is a blood test that measures the level of human chorionic gonadotropin (hCG) in a woman’s blood. This hormone is produced by the developing placenta after a fertilized egg implants in the uterus. A positive beta test indicates pregnancy, and doctors often perform two or more tests to monitor hCG levels and ensure they are rising appropriately.
Are home pregnancy tests accurate after IVF?
Home pregnancy tests can be accurate after IVF if used at the appropriate time. It is recommended to wait at least 14 days after the embryo transfer before taking a home pregnancy test. This allows enough time for hCG levels to rise and be detectable in urine. However, a blood test (beta hCG) performed by a healthcare provider is considered more accurate and can detect pregnancy earlier.
Can you get a false negative pregnancy test after IVF?
Yes, it is possible to get a false negative pregnancy test after IVF if the test is taken too early. hCG levels may not be high enough to be detected by a urine pregnancy test in the first few days following an embryo transfer. Waiting at least 14 days after the transfer and using a blood test (beta hCG) can help improve the accuracy of pregnancy detection.
Can an insurance company ask for a CCCT Test (Clomiphene Citrate Challenge Test) during IVF?
Insurance companies may require certain tests to determine coverage eligibility for fertility treatments, including IVF. The Clomiphene Citrate Challenge Test (CCCT) is a test that assesses ovarian reserve and may be requested by insurance providers to determine whether a woman meets the criteria for coverage. It is important to review your specific insurance policy and consult with your healthcare provider to understand the requirements and any necessary testing.
Do IVF babies look like Mom or Dad?
IVF babies inherit physical traits from both parents, just like babies conceived naturally. The appearance of an IVF baby is determined by the combination of genes from the egg and sperm used during the fertilization process.
Do IVF babies have 3 parents?
In most cases, IVF babies have two genetic parents, the egg and sperm donors. However, in the case of mitochondrial replacement therapy (MRT), the baby may have genetic material from three people. MRT involves replacing the mitochondria in a mother’s egg with healthy mitochondria from a donor egg. The resulting baby inherits nuclear DNA from the mother, father, and mitochondrial DNA from the egg donor. This technique is rare and primarily used to prevent the transmission of mitochondrial diseases.
How does IVF pick gender?
Gender selection can be achieved through IVF by using preimplantation genetic testing for aneuploidy (PGT-A) to determine the sex of embryos before transfer. PGT-A can identify whether embryos have XX (female) or XY (male) sex chromosomes, allowing parents and doctors to choose embryos of the desired gender for transfer.
What is the age limit for IVF in the USA?
There is no federal age limit for IVF in the USA. However, individual fertility clinics may have their own age restrictions based on their clinical experience and success rates. Generally, the chances of successful IVF treatment decrease with age, particularly after the age of 40.
Can you do IVF even if you are fertile?
Yes, IVF can be performed even if you are fertile. Some couples may choose to undergo IVF for various reasons, including genetic screening of embryos, gender selection, or fertility preservation for future family planning.
Do IVF babies have more health issues?
Yes, it is possible for IVF babies to have a slightly higher risk of certain health issues compared to naturally conceived babies. Some studies have shown a small increase in the risk of preterm birth, low birth weight, and birth defects in IVF babies. However, it is essential to note that the overall risk remains low, and the majority of IVF babies are born healthy.
Cost & Insurance
How much does a fertility test cost in the USA?
The cost of fertility testing in the USA varies depending on the specific tests being performed and whether they are covered by insurance. On average, basic fertility tests can range from a few hundred to a few thousand dollars. More advanced testing or specialized procedures, such as hysterosalpingograms or laparoscopies, can increase the cost.
Is IVF covered by insurance in the USA?
IVF coverage by insurance in the USA varies greatly depending on the insurance provider, specific policy, and state regulations. Some states have mandated fertility treatment coverage, including IVF, while others have no such requirements. It is crucial to review your insurance policy and consult with your healthcare provider to determine whether IVF is covered and what out-of-pocket costs you may be responsible for.
How much does it cost to test embryos?
The exact cost may vary from one clinic to another, from one test to another. However, the cost of testing embryos, such as PGT-A, could range from $3,000 to $5,000 on average. This is in addition to the standard IVF treatment costs.
How much does PGS testing cost in IVF?
Preimplantation genetic screening (PGS) testing in IVF, now commonly referred to as PGT-A, can cost anywhere from $3,000 to $5,000 on average. This cost is in addition to the standard IVF treatment costs and may vary depending on the clinic and the specific test being performed.