Unusual Cancers of Childhood Treatment (PDQ®): Treatment – Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
General Information About Unusual Cancers of Childhood
Unusual cancers of childhood are cancers rarely seen in children.
Cancer in children and adolescents is rare. Since 1975, the number of new cases of childhood cancer has slowly increased. Since 1975, the number of deaths from childhood cancer has decreased by more than half.
The unusual cancers discussed in this summary are so rare that most children’s hospitals are likely to see less than a handful of some types in several years. Because the unusual cancers are so rare, there is not a lot of information about what treatment works best. A child’s treatment is often based on what has been learned from treating other children. Sometimes, information is available only from reports of the diagnosis, treatment, and follow-up of one child or a small group of children who were given the same type of treatment.
Many different cancers are covered in this summary. They are grouped by where they are found in the body.
Tests are used to detect (find), diagnose, and stage unusual cancers of childhood.
Tests are done to detect, diagnose, and stage cancer. The tests used depend on the type of cancer. After cancer is diagnosed, tests are done to find out if cancer cells have spread from where the cancer began to other parts of the body. The process used to find out if cancer cells have spread to other parts of the body is called staging. The information gathered from the staging process determines the stage of the disease. It is important to know the stage in order to plan the best treatment.
The following tests and procedures may be used to detect, diagnose, and stage cancer:
- Physical exam and health history: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient’s health habits and past illnesses and treatments will also be taken.
- Blood chemistry studies: A procedure in which a blood sample is checked to measure the amounts of certain substances released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease.
- X-ray: An x-ray is a type of energy beam that can go through the body and onto film.
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an x-ray machine. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
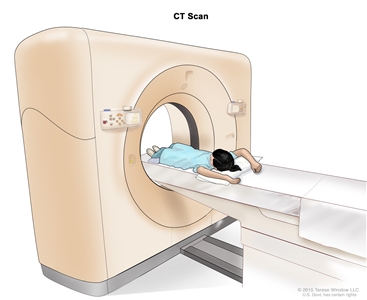
Computed tomography (CT) scan of the abdomen. The child lies on a table that slides through the CT scanner, which takes x-ray pictures of the inside of the abdomen. - PET scan (positron emission tomography scan): A procedure to find malignant tumor cells in the body. A small amount of radioactive glucose (sugar) is injected into a vein. The PET scanner rotates around the body and makes a picture of where glucose is being used in the body. Malignant tumor cells show up brighter in the picture because they are more active and take up more glucose than normal cells do.
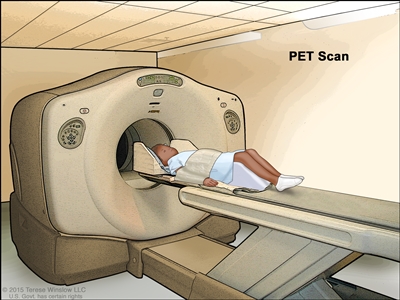
Positron emission tomography (PET) scan. The child lies on a table that slides through the PET scanner. The head rest and white strap help the child lie still. A small amount of radioactive glucose (sugar) is injected into the child’s vein, and a scanner makes a picture of where the glucose is being used in the body. Cancer cells show up brighter in the picture because they take up more glucose than normal cells do. - MRI (magnetic resonance imaging): A procedure that uses a magnet and radio waves to make a series of detailed pictures of areas inside the body. The pictures are made by a computer. This procedure is also called nuclear magnetic resonance imaging (NMRI).
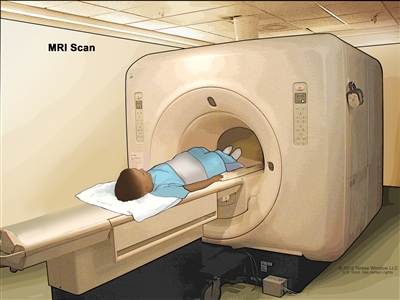
Magnetic resonance imaging (MRI) of the abdomen. The child lies on a table that slides into the MRI scanner, which takes pictures of the inside of the body. The pad on the child’s abdomen helps make the pictures clearer. - Ultrasound exam: A procedure in which high-energy sound waves (ultrasound) are bounced off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. The picture can be printed to be looked at later.
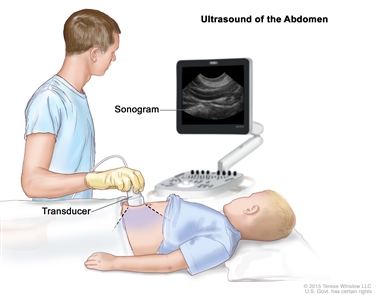
Abdominal ultrasound. An ultrasound transducer connected to a computer is pressed against the skin of the abdomen. The transducer bounces sound waves off internal organs and tissues to make echoes that form a sonogram (computer picture). - Endoscopy: A procedure to look at organs and tissues inside the body to check for abnormal areas. An endoscope is inserted through an incision (cut) in the skin or opening in the body, such as the mouth or rectum. An endoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of disease.
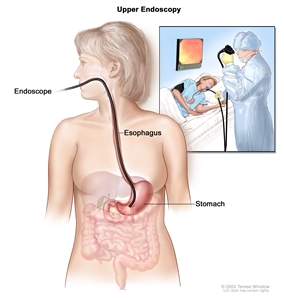
Upper endoscopy. A thin, lighted tube is inserted through the mouth to look for abnormal areas in the esophagus, stomach, and first part of the small intestine. - Bone scan: A procedure to check if there are rapidly dividing cells, such as cancer cells, in the bone. A very small amount of radioactive material is injected into a vein and travels through the bloodstream. The radioactive material collects in the bones with cancer and is detected by a scanner.
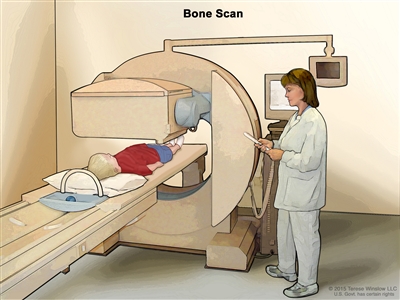
Bone scan. A small amount of radioactive material is injected into the child’s vein and travels through the blood. The radioactive material collects in the bones. As the child lies on a table that slides under the scanner, the radioactive material is detected and images are made on a computer screen. - Biopsy: The removal of cells or tissues so they can be viewed under a microscope by a pathologist to check for signs of cancer. There are many different types of biopsy procedures. The most common types include the following:
- Fine-needle aspiration (FNA) biopsy: The removal of tissue or fluid using a thin needle.
- Core biopsy: The removal of tissue using a wide needle.
- Incisional biopsy: The removal of part of a lump or a sample of tissue that doesn’t look normal.
- Excisional biopsy: The removal of an entire lump or area of tissue that doesn’t look normal.
There are three ways that cancer spreads in the body.
Cancer can spread through tissue, the lymph system, and the blood:
- Tissue. The cancer spreads from where it began by growing into nearby areas.
- Lymph system. The cancer spreads from where it began by getting into the lymph system. The cancer travels through the lymph vessels to other parts of the body.
- Blood. The cancer spreads from where it began by getting into the blood. The cancer travels through the blood vessels to other parts of the body.
Cancer may spread from where it began to other parts of the body.
When cancer spreads to another part of the body, it is called metastasis. Cancer cells break away from where they began (the primary tumor) and travel through the lymph system or blood.
- Lymph system. The cancer gets into the lymph system, travels through the lymph vessels, and forms a tumor (metastatic tumor) in another part of the body.
- Blood. The cancer gets into the blood, travels through the blood vessels, and forms a tumor (metastatic tumor) in another part of the body.
The metastatic tumor is the same type of cancer as the primary tumor. For example, if thyroid cancer spreads to the lung, the cancer cells in the lung are actually thyroid cancer cells. The disease is metastatic thyroid cancer, not lung cancer.
Treatment Option Overview
There are different types of treatment for children with unusual cancers.
Different types of treatments are available for children with cancer. Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment.
Because cancer in children is rare, taking part in a clinical trial should be considered. Some clinical trials are open only to patients who have not started treatment.
Children with unusual cancers should have their treatment planned by a team of health care providers who are experts in treating cancer in children.
Treatment will be overseen by a pediatric oncologist, a doctor who specializes in treating children with cancer. The pediatric oncologist works with other pediatric health care providers who are experts in treating children with cancer and who specialize in certain areas of medicine. These may include the following specialists:
- Pediatrician.
- Pediatric surgeon.
- Pediatric hematologist.
- Radiation oncologist.
- Pediatric nurse specialist.
- Rehabilitation specialist.
- Endocrinologist.
- Social worker.
- Psychologist.
Nine types of standard treatment are used:
Surgery
Surgery is a procedure used to find out whether cancer is present, to remove cancer from the body, or to repair a body part. Palliative surgery is done to relieve symptoms caused by cancer. Surgery is also called an operation.
After the doctor removes all the cancer that can be seen at the time of the surgery, some patients may be given chemotherapy or radiation therapy after surgery to kill any cancer cells that are left. Treatment given after the surgery, to lower the risk that the cancer will come back, is called adjuvant therapy.
Radiation therapy
Radiation therapy is a cancer treatment that uses high energy x-rays or other types of radiation to kill cancer cells or keep them from growing. There are different types of radiation therapy:
- External radiation therapy uses a machine outside the body to send radiation toward the cancer.
Proton beam radiation therapy is a type of high-energy, external radiation therapy. A radiation therapy machine aims streams of protons (tiny, invisible, positively-charged particles) at the cancer cells to kill them. This type of treatment causes less damage to nearby healthy tissue.
- Internal radiation therapy uses a radioactive substance that is injected into the body or sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer.
- 131I-MIBG (radioactive iodine) therapy is a type of internal radiation therapy used to treat pheochromocytoma and paraganglioma. Radioactive iodine is given by infusion. It enters the bloodstream and collects in certain kinds of tumor cells, killing them with the radiation that is given off.
The way the radiation therapy is given depends on the type of cancer being treated.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can affect cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly into the cerebrospinal fluid, a body cavity such as the abdomen, or an organ, the drugs mainly affect cancer cells in those areas. Combination chemotherapy is treatment using more than one anticancer drug. The way the chemotherapy is given depends on the type and stage of the cancer being treated.
High-dose chemotherapy with autologous stem cell rescue
High doses of chemotherapy are given to kill cancer cells. Healthy cells, including blood -forming cells, are also destroyed by the cancer treatment. Stem cell rescue is a treatment to replace the blood-forming cells. Stem cells (immature blood cells) are removed from the blood or bone marrow of the patient and are frozen and stored. After the patient completes chemotherapy, the stored stem cells are thawed and given back to the patient through an infusion. These reinfused stem cells grow into (and restore) the body’s blood cells.
Hormone therapy
Hormone therapy is a cancer treatment that removes hormones or blocks their action and stops cancer cells from growing. Hormones are substances that are made by glands in the body and flow through the bloodstream. Some hormones can cause certain cancers to grow. If tests show that the cancer cells have places where hormones can attach (receptors), drugs, surgery, or radiation therapy is used to reduce the production of hormones or block them from working. Hormone therapy with drugs called corticosteroids may be used to treat thymoma or thymic carcinoma.
Hormone therapy with a somatostatin analogue (octreotide or lanreotide) may be used to treat neuroendocrine tumors that have spread or cannot be removed by surgery. Octreotide may also be used to treat thymoma that does not respond to other treatment. This treatment stops extra hormones from being made by the neuroendocrine tumor. Octreotide or lanreotide are somatostatin analogues which are injected under the skin or into the muscle. Sometimes a small amount of a radioactive substance is attached to the drug and the radiation also kills cancer cells. This is called peptide receptor radionuclide therapy.
Immunotherapy
Immunotherapy is a treatment that uses the patient’s immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body’s natural defenses against cancer. This type of cancer treatment is also called biotherapy or biologic therapy.
- Interferon: Interferon affects the division of cancer cells and can slow tumor growth. It is used to treat nasopharyngeal cancer and papillomatosis.
- Epstein-Barr virus (EBV)-specific cytotoxic T-lymphocytes: White blood cells (T-lymphocytes) are treated in the laboratory with Epstein-Barr virus and then given to the patient to stimulate the immune system and fight cancer. EBV-specific cytotoxic T-lymphocytes are being studied for the treatment of nasopharyngeal cancer.
- Vaccine therapy: A cancer treatment that uses a substance or group of substances to stimulate the immune system to find the tumor and kill it. Vaccine therapy is used to treat papillomatosis.
- Immune checkpoint inhibitor therapy: Some types of immune cells, such as T cells, and some cancer cells have certain proteins, called checkpoint proteins, on their surface that keep immune responses in check. When cancer cells have large amounts of these proteins, they will not be attacked and killed by T cells. Immune checkpoint inhibitors block these proteins and the ability of T cells to kill cancer cells is increased.
There are two types of immune checkpoint inhibitor therapy:
- CTLA-4 is a protein on the surface of T cells that helps keep the body’s immune responses in check. When CTLA-4 attaches to another protein called B7 on a cancer cell, it stops the T cell from killing the cancer cell. CTLA-4 inhibitors attach to CTLA-4 and allow the T cells to kill cancer cells. Ipilimumab is a type of CTLA-4 inhibitor. Ipilimumab may be considered for the treatment of high-risk melanoma that has been completely removed during surgery. Ipilimumab is also used with nivolumab to treat certain children with colorectal cancer.
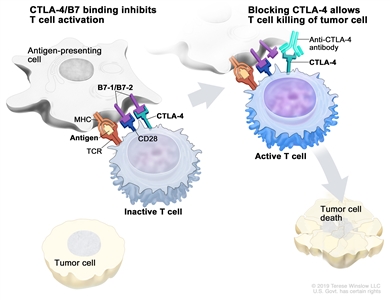
Immune checkpoint inhibitor. Checkpoint proteins, such as B7-1/B7-2 on antigen-presenting cells (APC) and CTLA-4 on T cells, help keep the body’s immune responses in check. When the T-cell receptor (TCR) binds to antigen and major histocompatibility complex (MHC) proteins on the APC and CD28 binds to B7-1/B7-2 on the APC, the T cell can be activated. However, the binding of B7-1/B7-2 to CTLA-4 keeps the T cells in the inactive state so they are not able to kill tumor cells in the body (left panel). Blocking the binding of B7-1/B7-2 to CTLA-4 with an immune checkpoint inhibitor (anti-CTLA-4 antibody) allows the T cells to be active and to kill tumor cells (right panel). - PD-1 is a protein on the surface of T cells that helps keep the body’s immune responses in check. When PD-1 attaches to another protein called PDL-1 on a cancer cell, it stops the T cell from killing the cancer cell. PD-1 inhibitors attach to PDL-1 and allow the T cells to kill cancer cells. Nivolumab is a type of PD-1 inhibitor. Nivolumab is used with ipilimumab to treat certain children with colorectal cancer.
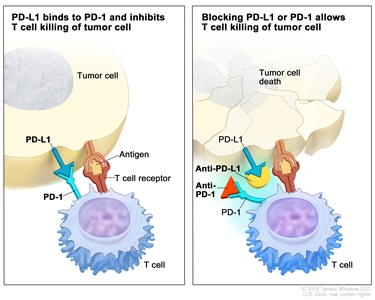
Immune checkpoint inhibitor. Checkpoint proteins, such as PD-L1 on tumor cells and PD-1 on T cells, help keep immune responses in check. The binding of PD-L1 to PD-1 keeps T cells from killing tumor cells in the body (left panel). Blocking the binding of PD-L1 to PD-1 with an immune checkpoint inhibitor (anti-PD-L1 or anti-PD-1) allows the T cells to kill tumor cells (right panel). immune checkpoint inhibitorsImmunotherapy uses the body’s immune system to fight cancer. This animation explains one type of immunotherapy that uses immune checkpoint inhibitors to treat cancer.
- CTLA-4 is a protein on the surface of T cells that helps keep the body’s immune responses in check. When CTLA-4 attaches to another protein called B7 on a cancer cell, it stops the T cell from killing the cancer cell. CTLA-4 inhibitors attach to CTLA-4 and allow the T cells to kill cancer cells. Ipilimumab is a type of CTLA-4 inhibitor. Ipilimumab may be considered for the treatment of high-risk melanoma that has been completely removed during surgery. Ipilimumab is also used with nivolumab to treat certain children with colorectal cancer.
Watchful waiting
Watchful waiting is closely monitoring a patient’s condition without giving any treatment until signs or symptoms appear or change. Watchful waiting may be used when the tumor is slow-growing or when it is possible the tumor may disappear without treatment.
Targeted therapy
Targeted therapy is a treatment that uses drugs or other substances to identify and attack specific cancer cells without harming normal cells. Types of targeted therapies used to treat unusual childhood cancers include the following:
- Tyrosine kinase inhibitors: These targeted therapy drugs block signals needed for tumors to grow. Vandetanib and cabozantinib are used to treat medullary thyroid cancer. Sunitinib is used to treat pheochromocytoma, paraganglioma, neuroendocrine tumors, thymoma, and thymic carcinoma. Crizotinib is used to treat tracheobronchial tumors.
- mTOR inhibitors: A type of targeted therapy that stops the protein that helps cells divide and survive. Everolimus is used to treat cardiac, neuroendocrine, and islet cell tumors.
- Monoclonal antibodies: This targeted therapy uses antibodies made in the laboratory, from a single type of immune system cell. These antibodies can identify substances on cancer cells or normal substances that may help cancer cells grow. The antibodies attach to the substances and kill the cancer cells, block their growth, or keep them from spreading. Monoclonal antibodies are given by infusion. They may be used alone or to carry drugs, toxins, or radioactive material directly to cancer cells. Bevacizumab is a monoclonal antibody used to treat papillomatosis.
- Histone methyltransferase inhibitors: This type of targeted therapy slows down the cancer cell’s ability to grow and divide. Tazemetostat is used to treat ovarian cancer. Tazemetostat is being studied in the treatment of chordomas that have recurred after treatment.
Targeted therapies are being studied in the treatment of other unusual cancers of childhood.
Embolization
Embolization is a treatment in which contrast dye and particles are injected into the hepatic artery through a catheter (thin tube). The particles block the artery, cutting off blood flow to the tumor. Sometimes a small amount of a radioactive substance is attached to the particles. Most of the radiation is trapped near the tumor to kill the cancer cells. This is called radioembolization.
New types of treatment are being tested in clinical trials.
This summary section describes treatments that are being studied in clinical trials. It may not mention every new treatment being studied. Information about clinical trials is available from the NCI website.
Gene therapy
Gene therapy is a treatment in which foreign genetic material (DNA or RNA) is inserted into a person’s cells to prevent or fight disease. Gene therapy is being studied in the treatment of papillomatosis.
Patients may want to think about taking part in a clinical trial.
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today’s standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Patients can enter clinical trials before, during, or after starting their cancer treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. Information about clinical trials supported by NCI can be found on NCI’s clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Follow-up tests may be needed.
Some of the tests that were done to diagnose the cancer or to find out the stage of the cancer may be repeated. Some tests will be repeated in order to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your child’s condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups.
Treatment for unusual cancers of childhood may cause side effects.
For information about side effects that begin during treatment for cancer, see our Side Effects page.
Side effects from cancer treatment that begin after treatment and continue for months or years are called late effects. Late effects of cancer treatment may include the following:
- Physical problems.
- Changes in mood, feelings, thinking, learning, or memory.
- Second cancers (new types of cancer).
Some late effects may be treated or controlled. It is important to talk with your child’s doctors about the possible late effects caused by some cancers and cancer treatments. (See the PDQ summary on Late Effects of Treatment for Childhood Cancer for more information).
Unusual Cancers of the Head and Neck
Nasopharyngeal Cancer
See the PDQ summary on Childhood Nasopharyngeal Cancer Treatment for more information.
Esthesioneuroblastoma
See the PDQ summary on Childhood Esthesioneuroblastoma Treatment for more information.
Thyroid Tumors
See the PDQ summary on Childhood Thyroid Cancer Treatment for more information.
Oral Cavity Cancer
See the PDQ summary on Childhood Oral Cavity Cancer Treatment for more information.
Salivary Gland Tumors
See the PDQ summary on Childhood Salivary Gland Tumors Treatment for more information.
Laryngeal Cancer and Papillomatosis
See the PDQ summary on Childhood Laryngeal Tumors Treatment for more information.
Midline Tract Cancer withNUTGene Changes (NUTMidline Carcinoma)
See the PDQ summary on Childhood Midline Tract Carcinoma with NUT Gene Changes Treatment for more information.
Unusual Cancers of the Chest
Breast Cancer
Breast cancer is a disease in which malignant (cancer) cells form in the tissues of the breast. Breast cancer can occur in the breast tissue of both male and female children.
Breast cancer is the most common cancer among females aged 15 to 39 years; however, less than 5% of breast cancers occur in females in this age group. Breast cancer in this age group is more aggressive and more difficult to treat than in older women. Treatments for younger and older women are similar. Younger patients with breast cancer may have genetic counseling (a discussion with a trained professional about inherited diseases) and testing for family cancer syndromes. Also, the possible effects of treatment on fertility should be considered.
Most breast tumors in children are fibroadenomas, which are benign (not cancer). Rarely, these tumors become large phyllodes tumors (cancer) and begin to grow quickly. If a benign tumor begins to grow quickly, a fine-needle aspiration (FNA) biopsy or an excisional biopsy will be done. The tissues removed during the biopsy will be viewed under a microscope by a pathologist to check for signs of cancer.
Risk Factors, Signs, and Diagnostic and Staging Tests
The risk of breast cancer is increased by the following:
- Having a personal history of a type of cancer that may spread to the breast, such as leukemia, rhabdomyosarcoma, soft tissue sarcoma, or lymphoma.
- Past treatment for another cancer, such as Hodgkin lymphoma, with radiation therapy to the breast or chest.
Other risk factors for breast cancer include the following:
- A family history of breast cancer in a mother, father, sister, or brother.
- Inherited changes in the BRCA1 or BRCA2gene or in other genes that increase the risk of breast cancer.
Breast cancer may cause any of the following signs. Check with your child’s doctor if your child has any of the following:
- A lump or thickening in or near the breast or in the underarm area.
- A change in the size or shape of the breast.
- A dimple or puckering in the skin of the breast.
- A nipple turned inward into the breast.
- Fluid, other than breast milk, from the nipples, including blood.
- Scaly, red, or swollen skin on the breast, nipple, or areola (the dark area of skin that is around the nipple).
- Dimples in the breast that look like the skin of an orange, called peau d’orange.
Other conditions that are not breast cancer may cause these same signs.
Tests to diagnose and stage breast cancer may include the following:
- Physical exam and health history.
- MRI.
- Ultrasound.
- PET scan.
- Blood chemistry studies.
- X-ray of the chest.
- Biopsy.
See the General Information section for a description of these tests and procedures.
Other tests that may be used to diagnose breast cancer include the following:
- Clinical breast exam (CBE): An exam of the breast by a doctor or other health professional. The doctor will carefully feel the breast and under the arm for lumps or anything else that seems unusual.
- Mammogram: An x-ray of the breast. When treatment for another cancer included radiation therapy to the breast or chest, it is important to have a mammogram and MRI of the breast to check for breast cancer. These should be done beginning at age 25, or 10 years after finishing radiation therapy, whichever is later.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of benign breast tumors in children may include the following:
- Watchful waiting. These tumors may disappear without treatment.
- Surgery to remove the tumor.
Treatment of breast cancer in children may include the following:
- Surgery to remove the tumor, but not the whole breast. Radiation therapy may also be given.
Treatment of recurrent breast cancer in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
See the PDQ summary Breast Cancer Treatment for more information on the treatment of adolescents and young adults with breast cancer.
Lung Cancer
Lung cancer is a disease in which malignant cancer cells form in the tissue of the lung. The lungs are a pair of cone-shaped breathing organs in the chest. The lungs bring oxygen into the body as you breathe in. They release carbon dioxide, a waste product of the body’s cells, as you breathe out. Each lung has sections called lobes. The left lung has two lobes. The right lung is slightly larger and has three lobes. Two tubes called bronchi lead from the trachea (windpipe) to the right and left lungs. Tiny air sacs called alveoli and small tubes called bronchioles make up the inside of the lungs.
In children, most lung or airway tumors are malignant (cancer). The following are the most common primary lung or airway tumors:
- Tracheobronchial tumors.
- Pleuropulmonary blastoma.
This summary is not about cancer that has spread to the lungs from another part of the body.
Tracheobronchial Tumors
Tracheobronchial tumors begin in the inside lining of the trachea or bronchi. Most tracheobronchial tumors in children are benign and occur in the trachea or large bronchi (large airways of the lung). Sometimes, a slow-growing tracheobronchial tumor, such as inflammatory myofibroblastic tumor, becomes cancer that may spread to other parts of the body.
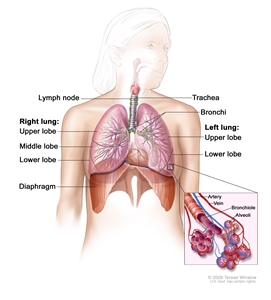
Anatomy of the respiratory system, showing the trachea and both lungs and their lobes and airways. Lymph nodes and the diaphragm are also shown. Oxygen is inhaled into the lungs and passes through the thin membranes of the alveoli and into the bloodstream (see inset).
Signs and Symptoms
Tracheobronchial tumors may cause any of the following signs and symptoms. Check with your child’s doctor if your child has any of the following:
- Dry cough.
- Wheezing.
- Trouble breathing.
- Spitting up blood from the airways or lung.
- Frequent infections in the lung, such as pneumonia.
- Feeling very tired.
- Loss of appetite or weight loss for no known reason.
Other conditions that are not tracheobronchial tumors may cause these same signs and symptoms. For example, symptoms of tracheobronchial tumors are a lot like the symptoms of asthma, which can make it hard to diagnose the tumor.
Diagnostic and Staging Tests
Tests to diagnose and stage tracheobronchial tumors may include the following:
- Physical exam and health history.
- X-ray of the chest.
- CT scan.
See the General Information section for a description of these tests and procedures.
A biopsy of the abnormal area is usually not done because it can cause severe bleeding.
Other tests used to diagnose tracheobronchial tumors include the following:
- Bronchography: A procedure to look inside the trachea and large airways in the lung for abnormal areas. A bronchoscope is inserted through the nose or mouth into the trachea and lungs. A bronchoscope is a thin, tube-like instrument with a light and a lens for viewing. A contrast dye is put through the bronchoscope to make the larynx, trachea, and airways show up more clearly on x-ray film.
- Octreotide scan: A type of radionuclide scan used to find tracheobronchial tumors or cancer that has spread to the lymph nodes. A very small amount of radioactive octreotide (a hormone that attaches to carcinoid tumors) is injected into a vein and travels through the bloodstream. The radioactive octreotide attaches to the tumor and a special camera that detects radioactivity is used to show where the tumors are in the body.
Prognosis
The prognosis (chance of recovery) for children with tracheobronchial cancer is very good, unless the child has rhabdomyosarcoma.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
The treatment of tracheobronchial tumors depends on the type of cell the cancer formed from. Treatment of tracheobronchial tumors in children may include the following:
- Surgery to remove the tumor. Sometimes a type of surgery called a sleeve resection is used. The lymph nodes and vessels where cancer has spread are also removed.
- Targeted therapy (crizotinib), for inflammatory myofibroblastic tumors that form in the trachea or bronchi.
- Chemotherapy and radiation therapy, for rhabdomyosarcoma that forms in the trachea or bronchi.
Treatment of recurrent tracheobronchial tumors in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
See the Neuroendocrine Tumors (Carcinoid Tumors) section of this summary for more information.
Pleuropulmonary Blastoma
Pleuropulmonary blastomas (PPBs) form in the tissue of the lung and pleura (tissue that covers the lungs and lines the inside of the chest). They can also form in the organs between the lungs including the heart, aorta, and pulmonary artery, or in the diaphragm (the main breathing muscle below the lungs). In most cases, PPBs are linked to a certain change in the DICER1gene.
There are three types of PPB:
- Type I tumors are cyst -like tumors in the lung. They are most common in children aged 2 years and younger and have a good chance of recovery. Type Ir tumors are Type I tumors that have regressed (gotten smaller) or have not grown or spread. After treatment, a Type I tumor may recur as a Type II or III tumor.
- Type II tumors are cyst-like with some solid parts. These tumors sometimes spread to the brain or other parts of the body.
- Type III tumors are solid tumors. These tumors often spread to the brain or other parts of the body.
Risk Factors, Signs and Symptoms, and Diagnostic and Staging Tests
The risk of PPB is increased by the following:
- Having a certain change in the DICER1 gene.
- Having a family history of DICER1 syndrome.
PPB may cause any of the following signs and symptoms. Check with your child’s doctor if your child has any of the following:
- A cough that doesn’t go away.
- Trouble breathing.
- Fever.
- Lung infections, such as pneumonia.
- Pain in the chest or abdomen.
- Loss of appetite.
- Weight loss for no known reason.
Other conditions that are not PPB may cause these same signs and symptoms.
Tests to diagnose and stage PPB may include the following:
- Physical exam and health history.
- X-ray of the chest.
- CT scan of the chest and abdomen.
- PET scan.
- MRI of the head.
- Bone scan.
See the General Information section for a description of these tests and procedures.
Other tests used to diagnose PPB include the following:
- Bronchoscopy: A procedure to look inside the trachea and large airways in the lung for abnormal areas. A bronchoscope is inserted through the nose or mouth into the trachea and lungs. A bronchoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue samples, which are checked under a microscope for signs of cancer.
- Thoracoscopy: A surgical procedure to look at the organs inside the chest to check for abnormal areas. An incision (cut) is made between two ribs, and a thoracoscope is inserted into the chest. A thoracoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of cancer. In some cases, this procedure is used to remove part of the esophagus or lung. If the thoracoscope cannot reach certain tissues, organs, or lymph nodes, a thoracotomy may be done. In this procedure, a larger incision is made between the ribs and the chest is opened.
PPBs may spread or recur (come back) even after being removed by surgery.
Prognosis
The prognosis (chance of recovery) depends on the following:
- The type of pleuropulmonary blastoma.
- Whether the tumor has spread to other parts of the body at the time of diagnosis.
- Whether the tumor was completely removed by surgery.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of pleuropulmonary blastoma in children includes the following:
- Surgery to remove the whole lobe of the lung the tumor is in, with or without chemotherapy.
Treatment of recurrent pleuropulmonary blastoma in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
Esophageal Tumors
Esophageal tumors may be benign (not cancer) or malignant (cancer). Esophageal cancer is a disease in which malignant cells form in the tissues of the esophagus. The esophagus is the hollow, muscular tube that moves food and liquid from the throat to the stomach. Most esophageal tumors in children begin in the thin, flat cells that line the inside of the esophagus.
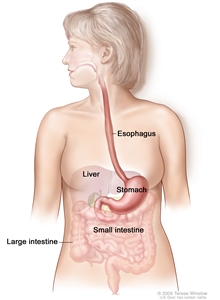
The esophagus and stomach are part of the upper gastrointestinal (digestive) system.
Risk Factors and Signs and Symptoms
The risk of esophageal cancer is increased by the following:
- Swallowing chemicals, which may burn the esophagus.
- Having gastroesophageal reflux.
- Having Barrett esophagus.
Esophageal cancer may cause any of the following signs and symptoms. Check with your child’s doctor if your child has any of the following:
- Trouble swallowing.
- Weight loss.
- Hoarseness and cough.
- Indigestion and heartburn.
- Vomiting with streaks of blood.
- Streaks of blood in sputum (mucus coughed up from the lungs).
Other conditions that are not esophageal cancer may cause these same signs and symptoms.
Diagnostic and Staging Tests
Tests to diagnose and stage esophageal cancer may include the following:
- Physical exam and health history.
- X-ray of the chest.
- CT scan.
- PET scan.
- MRI.
- Ultrasound.
See the General Information section for a description of these tests and procedures.
Other tests used to diagnose esophageal cancer include the following:
- Barium swallow: A series of x-rays of the esophagus and stomach. The patient drinks a liquid that contains barium (a silver-white metallic compound). The liquid coats the esophagus and stomach, and x-rays are taken. This procedure is also called an upper GI series.
- Esophagoscopy: A procedure to look inside the esophagus to check for abnormal areas. An esophagoscope is inserted through the mouth or nose and down the throat into the esophagus. An esophagoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue samples, which are checked under a microscope for signs of cancer. A biopsy is usually done during an esophagoscopy. Sometimes a biopsy shows changes in the esophagus that are not cancer but may lead to cancer.
- Bronchoscopy: A procedure to look inside the trachea and large airways in the lung for abnormal areas. A bronchoscope is inserted through the nose or mouth into the trachea and lungs. A bronchoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue samples, which are checked under a microscope for signs of cancer.
- Thoracoscopy: A surgical procedure to look at the organs inside the chest to check for abnormal areas. An incision (cut) is made between two ribs and a thoracoscope is inserted into the chest. A thoracoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of cancer. Sometimes this procedure is used to remove part of the esophagus or lung.
Prognosis
Esophageal cancer is hard to cure because it usually cannot be completely removed by surgery.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of esophageal cancer in children may include the following:
- Radiation therapy given through a plastic or metal tube placed through the mouth into the esophagus.
- Chemotherapy.
- Surgery to remove all or part of the tumor.
Treatment of recurrent esophageal cancer in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
See the PDQ summary on adult Esophageal Cancer for more information.
Thymoma
Thymoma is a tumor of the cells that cover the outside surface of the thymus. The thymus is a small organ in the upper chest under the breastbone. It is part of the lymph system and makes white blood cells, called lymphocytes, that help fight infection. Thymoma usually forms between the lungs in the front part of the chest and is often found during a chest x-ray that is done for another reason.
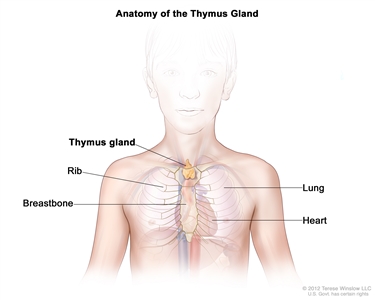
Anatomy of the thymus gland. The thymus gland is a small organ that lies in the upper chest under the breastbone. It makes white blood cells, called lymphocytes, which protect the body against infections.
The thymoma tumor cells look a lot like the normal cells of the thymus, grow slowly, and rarely spread beyond the thymus.
Other types of tumors, such as lymphoma or germ cell tumors, may form in the thymus but they are not considered to be thymoma.
Signs and Symptoms and Diagnostic and Staging Tests
Thymoma may cause any of the following signs and symptoms. Check with your child’s doctor if your child has any of the following:
- Coughing.
- Pain or a tight feeling in the chest.
- Trouble breathing.
- Trouble swallowing.
- Hoarseness.
- Fever.
- Weight loss.
- Superior vena cava syndrome.
Other conditions that are not thymoma may cause these same signs and symptoms.
People who develop thymoma often have one of the following immune system diseases or hormone disorders:
- Myasthenia gravis.
- Pure red cell aplasia.
- Hypogammaglobulinemia.
- Nephrotic syndrome.
- Scleroderma.
- Dermatomyositis.
- Lupus.
- Rheumatoid arthritis.
- Thyroiditis.
- Hyperthyroidism.
- Addison disease.
- Panhypopituitarism.
Tests to diagnose and stage thymoma may include the following:
- Physical exam and health history.
- X-ray of the chest.
- CT scan.
- PET scan.
- MRI.
- Biopsy.
See the General Information section for a description of these tests and procedures.
Prognosis
The prognosis (chance of recovery) is better when the tumor has not spread to other parts of the body. Childhood thymoma is usually diagnosed before the tumor has spread.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of thymoma in children may include the following:
- Surgery to remove as much of the tumor as possible.
- Radiation therapy, for tumors that cannot be removed by surgery or if tumor remains after surgery.
- Chemotherapy, for tumors that did not respond to other treatments.
- Hormone therapy (octreotide), for tumors that did not respond to other treatments.
- Targeted therapy (sunitinib), for tumors that did not respond to other treatments.
Treatment of recurrent thymoma in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
See the PDQ summary on adult Thymoma and Thymic Carcinoma Treatment for more information.
Thymic Carcinoma
Thymic carcinoma is a cancer of the cells that cover the outside surface of the thymus. The thymus is a small organ in the upper chest under the breastbone. It is part of the lymph system and makes white blood cells, called lymphocytes, that help fight infection. Thymic carcinoma usually forms between the lungs in the front part of the chest and is often found during a chest x-ray that is done for another reason.
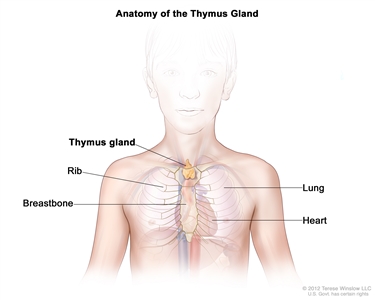
Anatomy of the thymus gland. The thymus gland is a small organ that lies in the upper chest under the breastbone. It makes white blood cells, called lymphocytes, which protect the body against infections.
The tumor cells in thymic carcinoma do not look like the normal cells of the thymus, grow more quickly, and are more likely to spread to other parts of the body.
Other types of tumors, such as lymphoma or germ cell tumors, may form in the thymus but they are not considered to be thymic carcinoma. (See the Thymoma section above for more information).
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Thymic carcinoma can rarely be completely removed by surgery and is likely to recur (come back) after treatment.
Treatment of thymic carcinoma in children may include the following:
- Surgery to remove as much of the tumor as possible.
- Radiation therapy, for tumors that cannot be removed by surgery or if tumor remains after surgery.
- Chemotherapy, for tumors that did not respond to radiation therapy.
- Targeted therapy (sunitinib), for tumors that did not respond to other treatments.
Treatment of recurrent thymic carcinoma in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
See the PDQ summary on adult Thymoma and Thymic Carcinoma Treatment for more information.
Heart Tumors
Most tumors that form in the heart are benign (not cancer). Benign heart tumors that may appear in children include the following:
- Rhabdomyoma: A tumor that forms in muscle made up of long fibers.
- Myxoma: A tumor that may be part of an inherited syndrome called Carney complex. (See the Multiple Endocrine Neoplasia Syndromes section for more information.)
- Teratomas: A type of germ cell tumor. In the heart, these tumors form most often in the pericardium (the sac that covers the heart). Some teratomas are malignant (cancer).
- Fibroma: A tumor that forms in fiber -like tissue that holds bones, muscles, and other organs in place.
- Histiocytoid cardiomyopathy tumor: A tumor that forms in the heart cells that control heart rhythm.
- Hemangiomas: A tumor that forms in the cells that line blood vessels.
- Neurofibroma: A tumor that forms in the cells and tissues that cover nerves.
Before birth and in newborns, the most common benign heart tumors are teratomas. An inherited condition called tuberous sclerosis can cause heart tumors to form in an unborn baby (fetus) or newborn.
Malignant tumors that begin in the heart are even more rare than benign heart tumors in children. Malignant heart tumors include:
- Malignant teratoma.
- Lymphoma.
- Rhabdomyosarcoma: A cancer that forms in muscle made up of long fibers.
- Angiosarcoma: A cancer that forms in cells that line blood vessels or lymph vessels.
- Undifferentiated pleomorphic sarcoma: A cancer that usually forms in the soft tissue, but it may also form in bone.
- Leiomyosarcoma: A cancer that forms in smooth muscle cells.
- Chondrosarcoma: A cancer that usually forms in bone cartilage but very rarely can begin in the heart.
- Synovial sarcoma: A cancer that usually forms around joints but may very rarely form in the heart or sac around the heart.
- Infantile fibrosarcoma: A cancer that forms in fiber-like tissue that holds bones, muscles, and other organs in place.
Signs and Symptoms
Heart tumors may cause any of the following signs and symptoms. Check with your child’s doctor if your child has any of the following:
- Change in the heart’s normal rhythm.
- Trouble breathing, especially when the child is lying down.
- Pain or tightness in the middle of the chest that feels better when the child is sitting up.
- Coughing.
- Fainting.
- Feeling dizzy, tired, or weak.
- Fast heart rate.
- Swelling in the legs, ankles, or abdomen.
- Feeling anxious.
- Signs of a stroke.
- Sudden numbness or weakness of the face, arm, or leg (especially on one side of the body).
- Sudden confusion or trouble speaking or understanding.
- Sudden trouble seeing with one or both eyes.
- Sudden trouble walking or feeling dizzy.
- Sudden loss of balance or coordination.
- Sudden severe headache for no known reason.
Sometimes heart tumors do not cause any signs or symptoms.
Other conditions that are not heart tumors may cause these same signs and symptoms.
Diagnostic and Staging Tests
Tests to diagnose and stage heart tumors may include the following:
- Physical exam and health history.
- X-ray of the chest.
- CT scan.
- MRI of the heart.
See the General Information section for a description of these tests and procedures.
Other tests used to diagnose or stage heart tumors include the following:
- Echocardiogram: A procedure in which high-energy sound waves (ultrasound) are bounced off the heart and nearby tissues or organs and make echoes. A moving picture is made of the heart and heart valves as blood is pumped through the heart.
- Electrocardiogram (EKG): A recording of the heart’s electrical activity to check its rate and rhythm. A number of small pads (electrodes) are placed on the patient’s chest, arms, and legs, and are connected by wires to the EKG machine. Heart activity is then recorded as a line graph on paper. Electrical activity that is faster or slower than normal may be a sign of heart disease or damage.
- Cardiac catheterization: A procedure to look inside the blood vessels and heart for abnormal areas or cancer. A long, thin, catheter is inserted into an artery or vein in the groin, neck, or arm and threaded through the blood vessels to the heart. A sample of tissue may be removed using a special tool. A pathologist views the tissue under a microscope to look for cancer cells.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of heart tumors in children may include the following:
- Watchful waiting, for rhabdomyoma, which sometimes shrinks and goes away on its own.
- Targeted therapy (everolimus) for patients who have rhabdomyoma and tuberous sclerosis.
- Chemotherapy followed by surgery (which may include removing some or all of the tumor or a heart transplant), for sarcomas.
- Surgery alone, for other tumor types.
- Radiation therapy for tumors that cannot be removed by surgery.
Treatment of recurrent heart tumors in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
Mesothelioma
Malignant mesothelioma is a disease in which malignant (cancer) cells are found in the following:
- Pleura: A thin layer of tissue that lines the chest cavity and covers the lungs.
- Peritoneum: A thin layer of tissue that lines the abdomen and covers most of the organs in the abdomen.
- Pericardium: A thin layer of tissue that surrounds the heart.
The tumors often spread over the surface of organs without spreading into the organ. They may spread to nearby lymph nodes or in other parts of the body. Malignant mesothelioma may also form in the testicles, but this is rare.
Risk Factors and Signs and Symptoms
Mesothelioma is sometimes a late effect of treatment for an earlier cancer, especially after treatment with radiation therapy. In adults, mesothelioma is linked to being exposed to asbestos, which was once used as building insulation. There is no information about the risk of mesothelioma in children exposed to asbestos.
Mesothelioma may cause any of the following signs and symptoms. Check with your child’s doctor if your child has any of the following:
- Trouble breathing.
- Cough for no known reason.
- Pain under the rib cage or pain in the chest and abdomen.
- Weight loss for no known reason.
- Feeling very tired.
Other conditions that are not mesothelioma may cause these same signs and symptoms.
Diagnostic and Staging Tests
Tests to diagnose and stage mesothelioma may include the following:
- Physical exam and health history.
- X-ray of the chest.
- CT scan.
- PET scan.
- MRI.
- Fine-needle aspiration (FNA) biopsy.
See the General Information section for a description of these tests and procedures.
Other tests used to diagnose mesothelioma include the following:
- Pulmonary function test (PFT): A test to see how well the lungs are working. It measures how much air the lungs can hold and how quickly air moves into and out of the lungs. It also measures how much oxygen is used and how much carbon dioxide is given off during breathing. This is also called a lung function test.
- Bronchoscopy: A procedure to look inside the trachea and large airways in the lung for abnormal areas. A bronchoscope is inserted through the nose or mouth into the trachea and lungs. A bronchoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue samples, which are checked under a microscope for signs of cancer.
- Thoracoscopy: A surgical procedure to look at the organs inside the chest to check for abnormal areas. An incision (cut) is made between two ribs and a thoracoscope is inserted into the chest. A thoracoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of cancer. In some cases, this procedure is used to remove part of the esophagus or lung.
- Laparoscopy: A surgical procedure to look at the organs inside the abdomen to check for abnormal areas. Small incisions (cuts) are made in the wall of the abdomen and a laparoscope (thin, lighted tube) is inserted into one of the incisions. Other instruments may be inserted through the same or other incisions to perform procedures such as removing organs or taking tissue samples to be checked under a microscope for signs of cancer.
- Cytologic exam: An exam of cells under a microscope (by a pathologist) to check for anything abnormal. For mesothelioma, fluid is taken from around the lungs or from the abdomen. A pathologist checks the cells in the fluid.
Prognosis
The prognosis (chance of recovery) is better when the tumor has not spread to other parts of the body.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of mesothelioma in children may include the following:
- Surgery to remove the part of the chest lining with cancer and some of the healthy tissue around it.
- Chemotherapy.
- Radiation therapy, as palliative therapy, to relieve pain and improve quality of life.
Treatment of recurrent mesothelioma in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
See the PDQ summary on adult Malignant Mesothelioma Treatment for more information.
Unusual Cancers of the Abdomen
Adrenocortical Carcinoma
Adrenocortical carcinoma is a disease in which malignant (cancer) cells form in the outer layer of the adrenal gland. There are two adrenal glands. The adrenal glands are small and shaped like a triangle. One adrenal gland sits on top of each kidney. Each adrenal gland has two parts. The center of the adrenal gland is the adrenal medulla. The outer layer of the adrenal gland is the adrenal cortex. Adrenocortical carcinoma is also called cancer of the adrenal cortex.
Childhood adrenocortical carcinoma occurs most commonly in patients younger than 6 years or in the teen years, and more often in females.
The adrenal cortex makes important hormones that do the following:
- Balance the water and salt in the body.
- Help keep blood pressure normal.
- Help control the body’s use of protein, fat, and carbohydrates.
- Cause the body to have male or female characteristics.
Risk Factors, Signs and Symptoms, and Diagnostic and Staging Tests
The risk of adrenocortical carcinoma is increased by having a certain mutation (change) in a gene or any of the following syndromes:
- Li-Fraumeni syndrome.
- Beckwith-Wiedemann syndrome.
- Hemihypertrophy.
Adrenocortical carcinoma may cause any of the following signs and symptoms. Check with your child’s doctor if your child has any of the following:
- A lump in the abdomen.
- Pain in the abdomen or back.
- Feeling of fullness in the abdomen.
Also, a tumor of the adrenal cortex may be functioning (makes more hormones than normal) or nonfunctioning (does not make extra hormones). Most tumors of the adrenal cortex in children are functioning tumors. The extra hormones made by functioning tumors may cause certain signs or symptoms of disease and these depend on the type of hormone made by the tumor. For example, extra androgen hormone may cause both male and female children to develop masculine traits, such as body hair or a deep voice, grow faster, and have acne. Extra estrogen hormone may cause the growth of breast tissue in male children. Extra cortisol hormone may cause Cushing syndrome or hypercortisolism.
(See the PDQ summary on adult Adrenocortical Carcinoma Treatment for more information on the signs and symptoms of adrenocortical carcinoma.)
The tests and procedures used to diagnose and stage adrenocortical carcinoma depend on the patient’s symptoms. These tests and procedures may include the following:
- Physical exam and health history.
- Blood chemistry studies.
- X-ray of the chest, abdomen, or bones.
- CT scan.
- MRI.
- PET scan.
- Ultrasound.
- Biopsy (the mass is removed during surgery and then the sample is checked for signs of cancer).
See the General Information section for a description of these tests and procedures.
Other tests used to diagnose adrenocortical carcinoma include the following:
- Twenty-four-hour urine test: A test in which urine is collected for 24 hours to measure the amounts of cortisol or 17-ketosteroids. A higher than normal amount of these substances in the urine may be a sign of disease in the adrenal cortex.
- Low-dose dexamethasone suppression test: A test in which one or more small doses of dexamethasone are given. The level of cortisol is checked from a sample of blood or from urine that is collected for three days. This test is done to check if the adrenal gland is making too much cortisol.
- High-dose dexamethasone suppression test: A test in which one or more high doses of dexamethasone are given. The level of cortisol is checked from a sample of blood or from urine that is collected for three days. This test is done to check if the adrenal gland is making too much cortisol or if the pituitary gland is telling the adrenal glands to make too much cortisol.
- Blood hormone studies: A procedure in which a blood sample is checked to measure the amounts of certain hormones released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease in the organ or tissue that makes it. The blood may be checked for testosterone or estrogen. A higher than normal amount of these hormones may be a sign of adrenocortical carcinoma.
- Adrenal angiography: A procedure to look at the arteries and the flow of blood near the adrenal gland. A contrast dye is injected into the adrenal arteries. As the dye moves through the blood vessel, a series of x-rays are taken to see if any arteries are blocked.
- Adrenal venography: A procedure to look at the adrenal veins and the flow of blood near the adrenal glands. A contrast dye is injected into an adrenal vein. As the contrast dye moves through the vein, a series of x-rays are taken to see if any veins are blocked. A catheter (very thin tube) may be inserted into the vein to take a blood sample, which is checked for abnormal hormone levels.
Prognosis
The prognosis (chance of recovery) is good for patients who have small tumors that have been completely removed by surgery. For other patients, the prognosis depends on the following:
- Size of the tumor.
- How quickly the cancer is growing.
- Whether there are changes in certain genes.
- Whether the tumor has spread to other parts of the body, including the lymph nodes.
- Child’s age.
- Whether the covering around the tumor broke open during surgery to remove the tumor.
- Whether the tumor was completely removed during surgery.
- Whether the child has developed masculine traits.
Adrenocortical carcinoma can spread to the liver, lung, kidney, or bone.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of adrenocortical carcinoma in children may include the following:
- Surgery to remove the adrenal gland and, if needed, cancer that has spread to other parts of the body. Sometimes chemotherapy is also given.
Treatment of recurrent adrenocortical carcinoma in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
See the PDQ summary on adult Adrenocortical Carcinoma Treatment for more information.
Stomach (Gastric) Cancer
Stomach cancer is a disease in which malignant (cancer) cells form in the lining of the stomach. The stomach is a J-shaped organ in the upper abdomen. It is part of the digestive system, which processes nutrients (vitamins, minerals, carbohydrates, fats, proteins, and water) in foods that are eaten and helps pass waste material out of the body. Food moves from the throat to the stomach through a hollow, muscular tube called the esophagus. After leaving the stomach, partly-digested food passes into the small intestine and then into the large intestine.
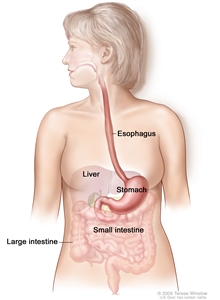
The esophagus and stomach are part of the upper gastrointestinal (digestive) system.
Risk Factors and Signs and Symptoms
The risk of stomach cancer is increased by the following:
- Having an infection with Helicobacter pylori (H. pylori)bacterium, which is found in the stomach.
- Having an inherited condition called familial diffuse gastric cancer.
Many patients do not have signs and symptoms until the cancer spreads. Stomach cancer may cause any of the following signs and symptoms. Check with your child’s doctor if your child has any of the following:
- Anemia (tiredness, dizziness, fast or irregular heartbeat, shortness of breath, pale skin).
- Stomach pain.
- Loss of appetite.
- Weight loss for no known reason.
- Nausea.
- Vomiting.
- Constipation or diarrhea.
- Weakness.
Other conditions that are not stomach cancer may cause these same signs and symptoms.
Diagnostic and Staging Tests
Tests to diagnose and stage stomach cancer may include the following:
- Physical exam and health history.
- X-ray of the abdomen.
- Blood chemistry studies.
- CT scan.
- Biopsy.
See the General Information section for a description of these tests and procedures.
Other tests used to diagnose and stage stomach cancer include the following:
- Upper endoscopy: A procedure to look inside the esophagus, stomach, and duodenum (first part of the small intestine) to check for abnormal areas. An endoscope is passed through the mouth and down the throat into the esophagus. An endoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of disease.
- Barium swallow: A series of x-rays of the esophagus and stomach. The patient drinks a liquid that contains barium (a silver-white metallic compound). The liquid coats the esophagus and stomach, and x-rays are taken. This procedure is also called an upper GI series.
- Complete blood count (CBC): A procedure in which a sample of blood is drawn and checked for the following:
- The number of red blood cells, white blood cells, and platelets.
- The amount of hemoglobin (the protein that carries oxygen) in the red blood cells.
- The portion of the blood sample made up of red blood cells.
Prognosis
Prognosis (chance of recovery) depends on whether the cancer has spread at the time of diagnosis and how well the cancer responds to treatment.
Stomach cancer may spread to the liver, lung, peritoneum, or to other parts of the body.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of stomach cancer in children may include the following:
- Surgery to remove the cancer and some healthy tissue around it.
- Surgery to remove as much of the cancer as possible, followed by radiation therapy and chemotherapy.
Treatment of recurrent stomach cancer in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
See the Gastrointestinal Stromal Tumors (GIST) section of this summary and the Neuroendocrine Tumors (Carcinoids) section of this summary for information about gastrointestinal carcinoids and neuroendocrine tumors.
Pancreatic Cancer
Pancreatic cancer is a disease in which malignant (cancer) cells form in the tissues of the pancreas. The pancreas is a pear-shaped gland about 6 inches long. The wide end of the pancreas is called the head, the middle section is called the body, and the narrow end is called the tail. Many different kinds of tumors can form in the pancreas. Some tumors are benign (not cancer).
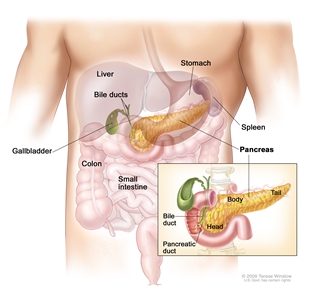
Anatomy of the pancreas. The pancreas has three areas: head, body, and tail. It is found in the abdomen near the stomach, intestines, and other organs.
The pancreas has two main jobs in the body:
- To make juices that help digest (break down) food. These juices are secreted into the small intestine.
- To make hormones that help control the sugar and salt levels in the blood. These hormones are secreted into the bloodstream.
There are four types of pancreatic cancer in children:
- Solid pseudopapillary tumor of the pancreas. This is the most common type of pancreatic tumor. It most commonly affects females that are older adolescents and young adults. These slow-growing tumors have both cyst -like and solid parts. Solid pseudopapillary tumor of the pancreas is unlikely to spread to other parts of the body and the prognosis is very good. Occasionally, the tumor may spread to the liver, lung, or lymph nodes.
- Pancreatoblastoma. It usually occurs in children aged 10 years or younger. Children with Beckwith-Wiedemann syndrome and familial adenomatous polyposis (FAP) syndrome have an increased risk of developing pancreatoblastoma. These slow-growing tumors often make the tumor marker alpha-fetoprotein. These tumors may also make adrenocorticotropic hormone (ACTH) and antidiuretic hormone (ADH). Pancreatoblastoma may spread to the liver, lungs, and lymph nodes. The prognosis for children with pancreatoblastoma is good.
- Islet cell tumors. These tumors are not common in children and can be benign or malignant. Islet cell tumors may occur in children with multiple endocrine neoplasia type 1 (MEN1) syndrome. The most common types of islet cell tumors are insulinomas and gastrinomas. Other types of islet cell tumors are ACTHoma and VIPoma. These tumors may make hormones, such as insulin, gastrin, ACTH, or ADH. When too much of a hormone is made, signs and symptoms of disease occur.
- Pancreatic carcinoma. Pancreatic carcinoma is very rare in children. The two types of pancreatic carcinoma are acinar cell carcinoma and ductal adenocarcinoma.
Signs and Symptoms
General signs and symptoms of pancreatic cancer may include the following:
- Fatigue.
- Weight loss for no known reason.
- Loss of appetite.
- Stomach discomfort.
- Lump in the abdomen.
In children, some pancreatic tumors do not secrete hormones and there are no signs and symptoms of disease. This makes it hard to diagnose pancreatic cancer early.
Pancreatic tumors that do secrete hormones may cause signs and symptoms. The signs and symptoms depend on the type of hormone being made.
If the tumor secretes insulin, signs and symptoms that may occur include the following:
- Low blood sugar. This can cause blurred vision, headache, and feeling lightheaded, tired, weak, shaky, nervous, irritable, sweaty, confused, or hungry.
- Changes in behavior.
- Seizures.
- Coma.
If the tumor secretes gastrin, signs and symptoms that may occur include the following:
- Stomach ulcers that keep coming back.
- Pain in the abdomen, which may spread to the back. The pain may come and go and it may go away after taking an antacid.
- The flow of stomach contents back into the esophagus (gastroesophageal reflux).
- Diarrhea.
Signs and symptoms caused by tumors that make other types of hormones, such as ACTH or ADH, may include the following:
- Watery diarrhea.
- Dehydration (feeling thirsty, making less urine, dry skin and mouth, headaches, dizziness, or feeling tired).
- Low sodium (salt) level in the blood (confusion, sleepiness, muscle weakness, and seizures).
- Weight loss or gain for no known reason.
- Round face and thin arms and legs.
- Feeling very tired and weak.
- High blood pressure.
- Purple or pink stretch marks on the skin.
Check with your child’s doctor if you see any of these problems in your child. Other conditions that are not pancreatic cancer may cause these same signs and symptoms.
Diagnostic and Staging Tests
Tests to diagnose and stage pancreatic cancer may include the following:
- Physical exam and health history.
- X-ray of the chest.
- CT scan.
- MRI.
- PET scan.
- Biopsy.
- Core-needle biopsy: The removal of tissue using a wide needle.
- Laparoscopy: A surgical procedure to look at the organs inside the abdomen to check for signs of disease. Small incisions (cuts) are made in the wall of the abdomen and a laparoscope (a thin, lighted tube) is inserted into one of the incisions. Other instruments may be inserted through the same or other incisions to perform procedures such as removing organs or taking tissue samples to be checked under a microscope for signs of disease.
- Laparotomy: A surgical procedure in which an incision (cut) is made in the wall of the abdomen to check the inside of the abdomen for signs of disease. The size of the incision depends on the reason the laparotomy is being done. Sometimes organs are removed or tissue samples are taken and checked under a microscope for signs of disease.
See the General Information section for a description of these tests and procedures.
Other tests used to diagnose pancreatic cancer include the following:
- Endoscopic ultrasound (EUS): A procedure in which an endoscope is inserted into the body, usually through the mouth or rectum. An endoscope is a thin, tube-like instrument with a light and a lens for viewing. A probe at the end of the endoscope is used to bounce high-energy sound waves (ultrasound) off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. This procedure is also called endosonography.
- Somatostatin receptor scintigraphy: A type of radionuclide scan used to find pancreatic tumors. A very small amount of radioactive octreotide (a hormone that attaches to carcinoid tumors) is injected into a vein and travels through the bloodstream. The radioactive octreotide attaches to the tumor and a special camera that detects radioactivity is used to show where the tumors are in the body. This procedure is used to diagnose islet cell tumors.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of solid pseudopapillary tumor of the pancreas in children may include the following:
- Surgery to remove the tumor.
- Chemotherapy for tumors that cannot be removed by surgery or have spread to other parts of the body.
Treatment of pancreatoblastoma in children may include the following:
- Surgery to remove the tumor. A Whipple procedure may be done for tumors in the head of the pancreas.
- Chemotherapy may be given to shrink the tumor before surgery. More chemotherapy may be given after surgery for large tumors, tumors that could not initially be removed by surgery, and tumors that have spread to other parts of the body.
- Chemotherapy may be given if the tumor does not respond to treatment or comes back.
Treatment of islet cell tumors in children may include drugs to treat symptoms caused by hormones and the following:
- Surgery to remove the tumor.
- Chemotherapy and targeted therapy (mTOR inhibitor therapy) for tumors that cannot be removed by surgery or that have spread to other parts of the body.
See the PDQ summary on adult Pancreatic Neuroendocrine Tumors (Islet Cell Tumors) Treatment for more information on pancreatic tumors.
There are few reported cases of pancreatic carcinoma in children. (See the PDQ summary on adult Pancreatic Cancer Treatment for possible treatment options.)
Treatment of recurrent pancreatic carcinoma in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
See the PDQ summaries on adult Pancreatic Cancer Treatment and adult Pancreatic Neuroendocrine Tumors (Islet Cell Tumors) Treatment for more information on pancreatic tumors.
Colorectal Cancer
Colorectal cancer is a disease in which malignant (cancer) cells form in the tissues of the colon or the rectum. The colon is part of the body’s digestive system. The digestive system removes and processes nutrients (vitamins, minerals, carbohydrates, fats, proteins, and water) from foods and helps pass waste material out of the body. The digestive system is made up of the esophagus, stomach, and the small and large intestines. The colon (large bowel) is the first part of the large intestine and is about 5 feet long. Together, the rectum and anal canal make up the last part of the large intestine and are 6-8 inches long. The anal canal ends at the anus (the opening of the large intestine to the outside of the body).
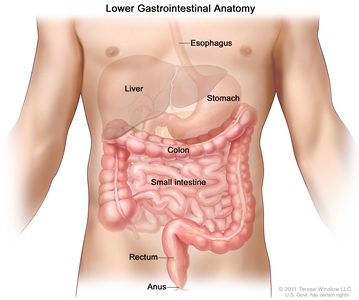
Anatomy of the lower digestive system, showing the colon and other organs.
Risk Factors, Signs and Symptoms, and Diagnostic and Staging Tests
Childhood colorectal cancer may be part of an inherited syndrome. Some colorectal cancers in young people are linked to a gene mutation that causes polyps (growths in the mucous membrane that lines the colon) to form that may turn into cancer later.
The risk of colorectal cancer is increased by having certain inherited conditions, such as:
- Familial adenomatous polyposis (FAP).
- Attenuated FAP.
- MUTYH-associated polyposis.
- Lynch syndrome.
- Oligopolyposis.
- Change in the NTHL1 gene.
- Juvenile polyposis syndrome.
- Cowden syndrome.
- Peutz-Jeghers syndrome.
- Neurofibromatosis type 1 (NF1).
Colon polyps that form in children who do not have an inherited syndrome are not linked to an increased risk of cancer.
Signs and symptoms of childhood colorectal cancer usually depend on where the tumor forms. Colorectal cancer may cause any of the following signs and symptoms. Check with your child’s doctor if your child has any of the following:
- Tumors of the rectum or lower colon may cause pain in the abdomen, constipation, or diarrhea.
- Tumors in the part of the colon on the left side of the body may cause:
- A lump in the abdomen.
- Weight loss for no known reason.
- Nausea and vomiting.
- Loss of appetite.
- Blood in the stool.
- Anemia (tiredness, dizziness, fast or irregular heartbeat, shortness of breath, pale skin).
- Tumors in the part of the colon on the right side of the body may cause:
- Pain in the abdomen.
- Blood in the stool.
- Constipation or diarrhea.
- Nausea or vomiting.
- Weight loss for no known reason.
Other conditions that are not colorectal cancer may cause these same signs and symptoms.
Tests to diagnose and stage colorectal cancer may include the following:
- Physical exam and health history.
- X-ray of the chest.
- CT scan of the chest, abdomen, and pelvis.
- PET scan.
- MRI.
- Bone scan.
- Biopsy.
Other tests used to diagnose colorectal cancer include the following:
- Colonoscopy: A procedure to look inside the rectum and colon for polyps, abnormal areas, or cancer. A colonoscope is inserted through the rectum into the colon. A colonoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove polyps or tissue samples, which are checked under a microscope for signs of cancer.
- Barium enema: A series of x-rays of the lower gastrointestinal tract. A liquid that contains barium (a silver-white metallic compound) is put into the rectum. The barium coats the lower gastrointestinal tract and x-rays are taken. This procedure is also called a lower GI series.
- Fecal occult blood test: A test to check stool (solid waste) for blood that can only be seen with a microscope. Small samples of stool are placed on special cards and returned to the doctor or laboratory for testing.
- Complete blood count (CBC): A procedure in which a sample of blood is drawn and checked for the following:
- The number of red blood cells, white blood cells, and platelets.
- The amount of hemoglobin (the protein that carries oxygen) in the red blood cells.
- The portion of the blood sample made up of red blood cells.
- Kidney function test: A test in which blood or urine samples are checked for the amounts of certain substances released by the kidneys. A higher or lower than normal amount of a substance can be a sign that the kidneys are not working the way they should. This is also called a renal function test.
- Liver function test: A blood test to measure the blood levels of certain substances released by the liver. A high or low level of certain substances can be a sign of liver disease.
- Carcinoembryonic antigen (CEA) assay: A test that measures the level of CEA in the blood. CEA is released into the bloodstream from both cancer cells and normal cells. When found in higher than normal amounts, it can be a sign of colorectal cancer or other conditions.
Prognosis
The prognosis (chance of recovery) depends on the following:
- Whether the entire tumor was removed by surgery.
- Whether the cancer has spread to other parts of the body, such as the lymph nodes, liver, pelvis, or ovaries.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of colorectal cancer in children may include the following:
- Surgery to remove the tumor if it has not spread.
- Radiation therapy and chemotherapy for tumors in the rectum or lower colon.
- Combination chemotherapy, for advanced colorectal cancer.
- Immunotherapy with immune checkpoint inhibitors (ipilimumab and nivolumab).
Treatment of recurrent colorectal cancer in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
Children with certain familial colorectal cancer syndromes may be treated with:
- Surgery to remove the colon before cancer forms.
- Medicine to decrease the number of polyps in the colon.
Neuroendocrine Tumors (Carcinoid Tumors)
Neuroendocrine cells can act like nerve cells or hormone -making cells. The cells are scattered throughout organs such as the lungs (tracheobronchial) or digestive tract.
Neuroendocrine tumors (including carcinoid tumors) usually form in the lining of the stomach or intestines (including the appendix), but they can form in other organs, such as the pancreas, lungs, or liver. These tumors are usually small, slow-growing, and benign (not cancer). Some neuroendocrine tumors are malignant (cancer) and spread to other places in the body.
Most neuroendocrine tumors in children form in the appendix (a pouch that sticks out from the first part of the large intestine near the end of the small intestine). The tumor is often found during surgery to remove the appendix.
See the Tracheobronchial tumors section of this summary for information on tracheobronchial carcinoid tumors.
Signs and Symptoms
Signs and symptoms of neuroendocrine tumors depend on where the tumor forms. Neuroendocrine tumors in the appendix may cause the following signs and symptoms:
- Abdominal pain, especially on the lower right side of the abdomen.
- Fever.
- Nausea and vomiting.
- Diarrhea.
Neuroendocrine tumors that are not in the appendix may release hormones and other substances. Carcinoid syndrome caused by the hormone serotonin and other hormones, may cause any of the following signs and symptoms. Check with your child’s doctor if your child has any of the following:
- Redness and a warm feeling in the face, neck, and upper chest.
- A fast heartbeat.
- Trouble breathing.
- Sudden drop in blood pressure (restlessness, confusion, weakness, dizziness, and pale, cool, and clammy skin).
- Diarrhea.
Other conditions that are not neuroendocrine tumors may cause these same signs and symptoms.
Diagnostic and Staging Tests
Tests that check for signs of cancer are used to diagnose and stage neuroendocrine tumors. They may include:
- Physical exam and health history.
- Blood chemistry studies.
- MRI.
- PET scan.
- CT scan.
- Ultrasound.
See the General Information section for a description of these tests and procedures.
Other tests used to diagnose neuroendocrine tumors include the following:
- Twenty-four-hour urine test: A test in which urine is collected for 24 hours to measure the amounts of certain substances, such as hormones. An unusual (higher or lower than normal) amount of a substance can be a sign of disease in the organ or tissue that makes it. The urine sample is checked to see if it contains 5-HIAA (a breakdown product of the hormone serotonin which may be made by carcinoid tumors). This test is used to help diagnose carcinoid syndrome.
- Somatostatin receptor scintigraphy: A type of radionuclide scan that may be used to find tumors. A very small amount of radioactive octreotide (a hormone that attaches to tumors) is injected into a vein and travels through the blood. The radioactive octreotide attaches to the tumor and a special camera that detects radioactivity is used to show where the tumors are in the body. This procedure is also called octreotide scan and SRS.
Prognosis
The prognosis for neuroendocrine tumors in the appendix in children is usually excellent after surgery to remove the tumor. Neuroendocrine tumors that are not in the appendix are usually larger or have spread to other parts of the body at the time of diagnosis and do not respond well to chemotherapy. Larger tumors are more likely to recur (come back).
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of neuroendocrine tumors in the appendix in children may include the following:
- Surgery to remove the appendix.
Treatment of neuroendocrine tumors that have spread to the large intestine, pancreas, or stomach is usually surgery. Treatment of tumors that cannot be removed by surgery, multiple tumors, or tumors that have spread may include the following:
- Embolization.
- Somatostatin analogue therapy (octreotide or lanreotide).
- Peptide receptor radionuclide therapy.
- Targeted therapy with a tyrosine kinase inhibitor (sunitinib) or an mTOR inhibitor (everolimus).
Treatment of recurrent neuroendocrine tumors in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
See the PDQ summary on adult Gastrointestinal Carcinoid Tumors Treatment for more information.
Gastrointestinal Stromal Tumors
Gastrointestinal stromal cell tumors (GIST) usually begin in cells in the wall of the stomach or intestines. GISTs may be benign (not cancer) or malignant (cancer). Childhood GISTs are more common in girls, and usually appear in the teen years.
Risk Factors and Signs and Symptoms
GISTs in children are not the same as GISTs in adults. Patients should be seen at centers that specialize in the treatment of GISTs and the tumors should be tested for genetic changes. A small number of children have tumors with genetic changes like those found in adult patients. The risk of GIST is increased by the following genetic disorders:
- Carney triad.
- Carney-Stratakis syndrome.
Most children with GIST have tumors in the stomach and develop anemia caused by bleeding. Signs and symptoms of anemia include the following:
- Tiredness.
- Dizziness.
- A fast or irregular heartbeat.
- Shortness of breath.
- Pale skin.
A lump in the abdomen or a blockage of the intestine (crampy pain in the abdomen, nausea, vomiting, diarrhea, constipation, and swelling of the abdomen) are also signs of GIST.
Other conditions that are not anemia caused by GIST may cause these same signs and symptoms.
Diagnostic and Staging Tests
Tests that check for signs of cancer are used to diagnose and stage GISTs. They may include:
- Physical exam and health history.
- MRI.
- CT scan.
- PET scan.
- X-ray of the abdomen.
- Biopsy.
- Fine-needle aspiration: The removal of tissue using a thin needle.
See the General Information section for a description of these tests and procedures.
Other tests used to diagnose GIST include the following:
- Endoscopy: A procedure to look at organs and tissues inside the body to check for abnormal areas. An endoscope is inserted through an incision (cut) in the skin or opening in the body, such as the mouth or anus. An endoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of disease.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment for children who have tumors with genetic changes like those found in adult patients is targeted therapy with a tyrosine kinase inhibitor (imatinib or sunitinib).
Treatment for children whose tumors do not show genetic changes may include the following:
- Surgery to remove the tumor. More surgery may be needed if intestinal obstruction or bleeding occurs.
Treatment of recurrent GIST in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
- A clinical trial of a new chemotherapy drug.
Unusual Cancers of the Reproductive and Urinary Systems
Bladder Cancer
Bladder cancer is a disease in which malignant (cancer) cells form in the tissues of the bladder. The bladder is a hollow organ in the lower part of the abdomen. It is shaped like a small balloon and has a muscle wall that allows it to get bigger or smaller. Tiny tubules in the kidneys filter and clean the blood. They take out waste products and make urine. The urine passes from each kidney through a long tube called a ureter into the bladder. The bladder holds the urine until it passes through the urethra and leaves the body.
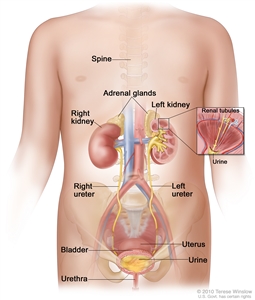
Anatomy of the female urinary system showing the kidneys, adrenal glands, ureters, bladder, and urethra. Urine is made in the renal tubules and collects in the renal pelvis of each kidney. The urine flows from the kidneys through the ureters to the bladder. The urine is stored in the bladder until it leaves the body through the urethra.
The most common type of bladder cancer is transitional cell cancer. Squamous cell and other more aggressive types of bladder cancer are less common.
Risk Factors, Signs and Symptoms, and Diagnostic and Staging Tests
The risk of bladder cancer is increased in children who have been treated for cancer with certain anticancer drugs, called alkylating agents, which includes cyclophosphamide, ifosfamide, busulfan, and temozolomide.
Bladder cancer may cause any of the following signs and symptoms. Check with your child’s doctor if your child has any of the following:
- Blood in the urine (slightly rusty to bright red in color).
- Frequent urination or feeling the need to urinate without being able to do so.
- Pain during urination.
- Abdominal or lower back pain.
Other conditions that are not bladder cancer may cause the same signs and symptoms.
Tests to diagnose and stage bladder cancer may include the following:
- Physical exam and health history.
- CT scan.
- Ultrasound of the bladder.
- Biopsy.
- Cystoscopy: A procedure to look inside the bladder and urethra to check for abnormal areas. A cystoscope is inserted through the urethra into the bladder. A cystoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue samples, which are checked under a microscope for signs of cancer. If a cystoscopy is not done at diagnosis, tissue samples are removed and checked for cancer during surgery to remove all or part of the bladder.
See the General Information section for a description of these tests and procedures.
Prognosis
In children, bladder cancer is usually low grade (not likely to spread) and the prognosis is usually excellent after surgery to remove the tumor.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of bladder cancer in children is usually the following:
- Surgery to remove part of the bladder. Transurethral resection (TUR) is a surgical procedure to remove tissue from the bladder using a resectoscope inserted into the bladder through the urethra. A resectoscope is a thin, tube-like instrument with a light, a lens for viewing, and a tool to remove tissue and burn away any remaining tumor cells. Tissue samples from the area where the tumor was removed are checked under a microscope for signs of cancer.
- Surgery to remove the bladder (rare).
Talk to your child’s doctor about how this type of surgery can affect urinating, sexual function, and fertility.
Treatment of recurrent bladder cancer in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
See the PDQ summary on adult Bladder Cancer Treatment for more information.
Testicular Cancer
Testicular cancer is a disease in which malignant (cancer) cells form in the tissues of one or both testicles. The testicles are 2 egg-shaped glands located inside the scrotum (a sac of loose skin that lies directly below the penis). The testicles are held within the scrotum by the spermatic cord, which also contains the vas deferens and vessels and nerves of the testicles.
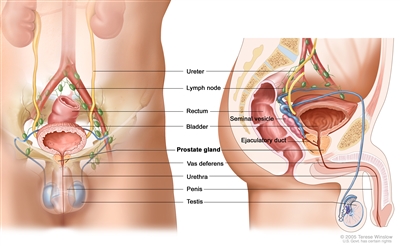
Anatomy of the male reproductive and urinary systems, showing the prostate, testicles, bladder, and other organs.
There are two types of testicular tumors:
- Germ cell tumors: Tumors that start in sperm cells in males. Testicular germ cell tumors may be benign (not cancer) or malignant (cancer). The most common testicular germ cell tumors in young boys are benign teratomas and malignant nonseminomas. Seminomas usually occur in young men and are rare in boys. See the PDQ summary on Childhood Extracranial Germ Cell Tumors Treatment for more information on testicular germ cell tumors.
- Non-germ cell tumors: Tumors that begin in the tissues that surround and support the testicles. These tumors may be benign or malignant. Juvenile granulosa cell tumors and Sertoli-Leydig cell tumors are two types of non-germ cell tumors.
Signs and Symptoms and Diagnostic and Staging Tests
Testicular cancer and its spread to other parts of the body may cause any of the following signs and symptoms. Check with your child’s doctor if your child has any of the following:
- Painless lump in the testicles.
- Early signs of puberty.
- Enlarged breasts.
A painless lump in the testicles may be a sign of a testicular tumor. Other conditions may also cause a lump in the testicles.
Tests to diagnose and stage non-germ cell testicular cancer may include the following:
- Physical exam and health history.
- CT scan of the chest, abdomen, or pelvis.
- MRI of the chest, abdomen, or pelvis.
- Ultrasound.
- Biopsy. The tissue removed during surgery is viewed under a microscope by a pathologist to check for signs of cancer.
See the General Information section for a description of these tests and procedures.
Other tests used to diagnose testicular tumors include the following:
- Serum tumor marker test: A procedure in which a sample of blood is examined to measure the amounts of certain substances released into the blood by organs, tissues, or tumor cells in the body. Certain substances are linked to specific types of cancer when found in increased levels in the blood. These are called tumor markers. The tumor marker alpha-fetoprotein is used to diagnose germ cell tumors.
Prognosis
In children, the prognosis is usually excellent after surgery to remove the tumor.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of non-germ cell testicular cancer in children may include the following:
- Surgery to remove the tumor from the testicle.
- Surgery to remove one or both testicles.
Treatment of recurrent non-germ cell testicular cancer in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
See the PDQ summary on Childhood Extracranial Germ Cell Tumors Treatment for more information on testicular germ cell tumors.
Ovarian Cancer
Ovarian cancer is a disease in which malignant (cancer) cells form in the ovary. The ovaries are a pair of organs in the female reproductive system. They are located in the pelvis, one on each side of the uterus (the hollow, pear-shaped organ where a fetus grows). Each ovary is about the size and shape of an almond in an adult woman. The ovaries produce eggs and female hormones (chemicals that control the way certain cells or organs function).
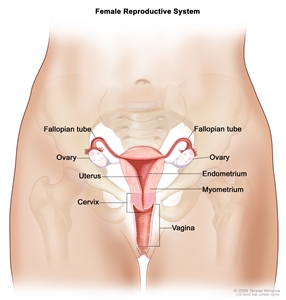
Anatomy of the female reproductive system. The organs in the female reproductive system include the uterus, ovaries, fallopian tubes, cervix, and vagina. The uterus has a muscular outer layer called the myometrium and an inner lining called the endometrium.
Most ovarian tumors in children are benign (not cancer). They occur most often in females aged 15 to 19 years.
There are several types of malignant (cancer) ovarian tumors:
- Germ cell tumors: Tumors that start in egg cells in females. These are the most common ovarian tumors in girls. (See the PDQ summary on Childhood Extracranial Germ Cell Tumors Treatment for more information on ovarian germ cell tumors.)
- Epithelial tumors: Tumors that start in the tissue covering the ovary. These are the second most common ovarian tumors in girls.
- Stromal tumors: Tumors that begin in stromal cells, which make up tissues that surround and support the ovaries. Juvenile granulosa cell tumors and Sertoli-Leydig cell tumors are two types of stromal tumors.
- Small cell carcinoma of the ovary: Cancer that begins in the ovary and may have spread to the abdomen, pelvis, or other parts of the body. This type of ovarian cancer is fast growing and has a poor prognosis.
Risk Factors, Signs and Symptoms, and Diagnostic and Staging Tests
The risk of ovarian cancer is increased by having one of the following conditions:
- Ollier disease (a disorder that causes abnormal growth of cartilage at the end of long bones).
- Maffucci syndrome (a disorder that causes abnormal growth of cartilage at the end of long bones and of blood vessels in the skin).
- Peutz-Jeghers syndrome (a disorder that causes polyps to form in the intestines and dark spots to form on the mouth and fingers).
- Pleuropulmonary blastoma syndrome (a disorder that may cause cystic nephroma, cysts in the lung, thyroid problems, and other cancers of the kidney, ovary, and soft tissue).
- DICER1 syndrome (a disorder that may cause goiter, polyps in the colon, and tumors of the ovary, cervix, testicle, kidney, brain, eye, and lining of the lung).
Ovarian cancer may cause any of the following signs and symptoms. Check with your child’s doctor if your child has any of the following:
- Pain or swelling in the abdomen.
- A lump in the abdomen.
- Constipation.
- Painful or missed menstrual periods.
- Unusual vaginal bleeding.
- Male sex traits, such as body hair or a deep voice.
- Early signs of puberty.
Other conditions that are not ovarian cancer may cause these same signs and symptoms.
Tests to diagnose and stage ovarian cancer may include the following:
- Physical exam and health history.
- CT scan.
- MRI.
- Ultrasound.
- Biopsy. The tissue removed during surgery is viewed under a microscope by a pathologist to check for signs of cancer.
See the General Information section for a description of these tests and procedures.
Other tests used to diagnose ovarian tumors include the following:
- Serum tumor marker test: A procedure in which a sample of blood is examined to measure the amounts of certain substances released into the blood by organs, tissues, or tumor cells in the body. Certain substances are linked to specific types of cancer when found in increased levels in the blood. These are called tumor markers. The tumor markers alpha-fetoprotein, beta-human chorionic gonadotropin (β-hCG), CEA, CA-125, and others are used to diagnose ovarian cancer.
During surgery to remove the tumor, fluid in the abdomen will be checked for signs of cancer.
Prognosis
Ovarian epithelial cancer is usually found at an early stage in children and is easier to treat than in adult patients.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of benign ovarian tumors in children may include the following:
- Surgery.
Treatment of ovarian epithelial cancer in children may include the following:
- Surgery.
- Radiation therapy.
- Chemotherapy.
Treatment of ovarian stromal tumors, including juvenile granulosa cell tumors and Sertoli-Leydig cell tumors, in children may include the following:
- Surgery to remove one ovary and one fallopian tube for early cancer.
- Surgery followed by chemotherapy for cancer that is advanced.
- Chemotherapy for cancer that has recurred (come back).
Treatment of small cell carcinoma of the ovary may include the following:
- Surgery followed by chemotherapy and high-dose chemotherapy with stem cell rescue.
- Targeted therapy (tazemetostat).
Treatment of recurrent ovarian cancer in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
See the following PDQ summaries for more information:
- Childhood Extracranial Germ Cell Tumors Treatment
- Ovarian Epithelial, Fallopian Tube, and Primary Peritoneal Cancer Treatment
- Ovarian Germ Cell Tumors Treatment
Cervical and Vaginal Cancer
Cervical cancer is a disease in which malignant (cancer) cells form in the cervix. The cervix is the lower, narrow end of the uterus (the hollow, pear-shaped organ where a baby grows). The cervix leads from the uterus to the vagina (birth canal). Vaginal cancer forms in the vagina. The vagina is the canal leading from the cervix to the outside of the body. At birth, a baby passes out of the body through the vagina (also called the birth canal).
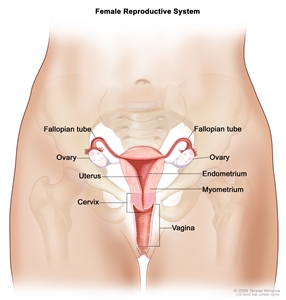
Anatomy of the female reproductive system. The organs in the female reproductive system include the uterus, ovaries, fallopian tubes, cervix, and vagina. The uterus has a muscular outer layer called the myometrium and an inner lining called the endometrium.
The most common sign of cervical and vaginal cancer is bleeding from the vagina. Other conditions may also cause vaginal bleeding. Children are often diagnosed with advanced disease.
Diagnostic and Staging Tests
Tests to diagnose and stage cervical and vaginal cancer may include the following:
- Physical exam and health history.
- Ultrasound.
- MRI.
- CT scan.
- Biopsy. A transvaginal needle biopsy is the removal of tissue using a needle that is guided by ultrasound.
- Bone scan.
See the General Information section for a description of these tests and procedures.
Other tests used to diagnose cervical and vaginal tumors include the following:
- Serum tumor marker test: A procedure in which a sample of blood is examined to measure the amounts of certain substances released into the blood by organs, tissues, or tumor cells in the body. Certain substances are linked to specific types of cancer when found in increased levels in the blood. These are called tumor markers.
- PAP test: A procedure to collect cells from the surface of the cervix and vagina. A piece of cotton, a brush, or a small wooden stick is used to gently scrape cells from the cervix and vagina. The cells are viewed under a microscope to find out if they are abnormal. This procedure is also called a Pap smear.
- Cystoscopy: A procedure to look inside the bladder and urethra to check for abnormal areas. A cystoscope is inserted through the urethra into the bladder. A cystoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue samples, which are checked under a microscope for signs of cancer.
- Proctoscopy: A procedure to look inside the rectum and anus to check for abnormal areas, using a proctoscope. A proctoscope is a thin, tube-like instrument with a light and a lens for viewing the inside of the rectum and anus. It may also have a tool to remove tissue samples, which are checked under a microscope for signs of cancer.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of childhood cervical and vaginal cancer may include the following:
- Surgery to remove as much of the cancer as possible, followed by radiation therapy, if cancer cells remain after surgery or cancer has spread to the lymph nodes.
- Chemotherapy may also be used but it is not yet known how well this treatment works.
Treatment of recurrent cervical and vaginal cancer in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
Other Rare Unusual Cancers of Childhood
Multiple Endocrine Neoplasia Syndromes
Multiple endocrine neoplasia (MEN) syndromes are inherited disorders that affect the endocrine system. The endocrine system is made up of glands and cells that make hormones and release them into the blood. MEN syndromes may cause hyperplasia (the growth of too many normal cells) or tumors that may be benign (not cancer) or malignant (cancer).
There are several types of MEN syndromes and each type may cause different conditions or cancers. Patients and family members with an increased risk of these syndromes should have genetic counseling and tests to check for the syndromes.
The two main types of MEN syndromes are MEN1 and MEN2:
| MEN1 syndrome is also called Werner syndrome. This syndrome usually causes tumors in the parathyroid gland, pituitary gland, and pancreas. Rarely, it causes tumors in the adrenal glands, gastrointestinal tract, fibrous tissue, and fat cells. The tumors make extra hormones and cause certain signs or symptoms of disease. The signs and symptoms depend on the type of hormone made by the tumor.
The most common sign of MEN1 syndrome is hypercalcemia. Hypercalcemia occurs when the parathyroid gland makes too much parathyroid hormone. Signs and symptoms of hypercalcemia include the following:
A diagnosis of MEN1 syndrome is usually made when tumors are found in two different places. The prognosis (chance of recovery) is usually good. Children who are diagnosed with MEN1 syndrome are checked for signs of cancer starting at age 5 and continuing for the rest of their life. Talk to your doctor about the tests and procedures that should be done to check for signs of cancer and how often they should be done. Children with MEN1 syndrome may also have primary hyperparathyroidism. In primary hyperparathyroidism, one or more of the parathyroid glands makes too much parathyroid hormone. The most common sign of primary hyperparathyroidism is kidney stones. Children with primary hyperparathyroidism may have genetic testing to check for gene changes linked to MEN1 syndrome. |
MEN2 syndrome includes three subgroups:
|
Tests used to diagnose and stage MEN syndromes depend on the signs and symptoms and the patient’s family history. They may include:
- Physical exam and history.
- Blood chemistry studies.
- Ultrasound.
- MRI.
- CT scan.
- PET scan.
- Fine-needle aspiration (FNA) or surgical biopsy.
See the General Information section for a description of these tests and procedures.
Other tests and procedures used to diagnose MEN syndromes include the following:
- Genetic testing: A laboratory test that analyzes cells or tissues to look for changes in a gene, chromosome, or protein. These changes may be a sign of a genetic disease or condition. They may also be linked to an increased risk of developing a specific disease or condition.
- Blood hormone studies: A procedure in which a blood sample is checked to measure the amounts of certain hormones released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease in the organ or tissue that makes it. The blood may be checked for abnormal levels of thyroid-stimulating hormone (TSH). TSH is made by the pituitary gland in the brain. It stimulates the release of thyroid hormone and controls how fast follicular thyroid cells grow. The blood may also be checked for high levels of the hormone calcitonin or parathyroid hormone (PTH).
- Radioactive iodine scan (RAI scan): A procedure to find areas in the body where thyroid cancer cells may be dividing quickly. Radioactive iodine (RAI) is used because only thyroid cells take up iodine. A very small amount of RAI is swallowed, travels through the blood, and collects in thyroid tissue and thyroid cancer cells anywhere in the body. Abnormal thyroid cells take up less iodine than normal thyroid cells do. Areas that do not take up the iodine normally are called cold spots. Cold spots show up lighter in the picture made by the scan. They can be either benign (not cancer) or malignant, so a biopsy is done to find out if they are cancer.
- Sestamibi scan: A type of radionuclide scan used to find an overactive parathyroid gland. A very small amount of a radioactive substance called technetium 99 is injected into a vein and travels through the bloodstream to the parathyroid gland. The radioactive substance will collect in the overactive gland and show up brightly on a special camera that detects radioactivity.
- Angiogram: A procedure to look at blood vessels and the flow of blood. A contrast dye is injected into a blood vessel. As the contrast dye moves through the blood vessel, x-rays are taken to see if there are any blockages.
- Venous sampling for an overactive parathyroid gland: A procedure in which a sample of blood is taken from veins near the parathyroid glands. The sample is checked to measure the amount of parathyroid hormone released into the blood by each gland. Venous sampling may be done if blood tests show there is an overactive parathyroid gland but imaging tests don’t show which one it is.
- Somatostatin receptor scintigraphy: A type of radionuclide scan that may be used to find tumors. A very small amount of radioactive octreotide (a hormone that attaches to tumors) is injected into a vein and travels through the blood. The radioactive octreotide attaches to the tumor and a special camera that detects radioactivity is used to show where the tumors are in the body. This procedure is also called octreotide scan and SRS.
- MIBG scan: A procedure used to find neuroendocrine tumors, such as pheochromocytoma. A very small amount of a substance called radioactive MIBG is injected into a vein and travels through the bloodstream. Neuroendocrine tumor cells take up the radioactive MIBG and are detected by a scanner. Scans may be taken over 1-3 days. An iodine solution may be given before or during the test to keep the thyroid gland from absorbing too much of the MIBG.
- Twenty-four-hour urine test: A test in which urine is collected for 24 hours to measure the amounts of catecholamines in the urine. Substances caused by the breakdown of these catecholamines are also measured. An unusual (higher- or lower-than-normal) amount of a substance can be a sign of disease in the organ or tissue that makes it. Higher-than-normal amounts may be a sign of pheochromocytoma.
- Pentagastrin stimulation test: A test in which blood samples are checked to measure the amount of calcitonin in the blood. Calcium gluconate and pentagastrin are injected into the blood and then several blood samples are taken over the next 5 minutes. If the level of calcitonin in the blood increases, it may be a sign of medullary thyroid cancer.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
There are several types of MEN syndrome, and each type may need different treatment:
- Patients with the MEN1 syndrome are treated for parathyroid, pancreatic and pituitary tumors.
- Patients with the MEN1 syndrome and primary hyperparathyroidism may have surgery to remove at least three parathyroid glands and the thymus.
- Patients with the MEN2A syndrome usually have surgery to remove the thyroid by age 5 or earlier if genetic tests show certain changes in the RET gene. The surgery is done to diagnose cancer or to prevent cancer from forming or spreading.
- Infants with the MEN2B syndrome may have surgery to remove the thyroid to prevent cancer.
- Children with the MEN2B syndrome who have medullary thyroid cancer may be treated with targeted therapy (kinase inhibitor).
- Patients with Hirschsprung disease and certain gene changes may have the thyroid removed to prevent cancer.
Treatment of recurrent MEN syndrome in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
Pheochromocytoma and Paraganglioma
Pheochromocytoma and paraganglioma are rare tumors that come from the same type of nerve tissue.
- Pheochromocytoma forms in the adrenal glands. There are two adrenal glands, one on top of each kidney in the back of the upper abdomen. Each adrenal gland has two parts. The outer layer of the adrenal gland is the adrenal cortex. The center of the adrenal gland is the adrenal medulla. Pheochromocytoma is a tumor of the adrenal medulla. The adrenal glands make important hormones called catecholamines. Adrenaline (epinephrine) and noradrenaline (norepinephrine) are two types of catecholamines that help control heart rate, blood pressure, blood sugar, and the way the body reacts to stress. Some pheochromocytomas release extra adrenaline and noradrenaline into the blood and cause symptoms.
- Paraganglioma forms outside the adrenal glands near the carotid artery, along nerve pathways in the head and neck, and in other parts of the body. Some paragangliomas make extra catecholamines called adrenaline and noradrenaline. The release of extra adrenaline and noradrenaline into the blood may cause symptoms.
Risk Factors, Signs and Symptoms, and Diagnostic and Staging Tests
Anything that increases your chance of getting a disease is called a risk factor. Having a risk factor doesn’t mean that you will get cancer; not having risk factors doesn’t mean that you will not get cancer. Talk with your child’s doctor if you think your child may be at risk.
The risk of pheochromocytoma or paraganglioma is increased by having any of the following inherited syndromes or gene changes:
- Multiple endocrine neoplasia type 1 (MEN1) syndrome.
- Multiple endocrine neoplasia type 2 syndrome (MEN2A and MEN2B).
- von Hippel-Lindau disease (VHL).
- Neurofibromatosis type 1 (NF1).
- Carney-Stratakis dyad (paraganglioma and gastrointestinal stromal tumor [GIST]).
- Carney triad (paraganglioma, GIST, and pulmonary chondroma).
- Changes in certain genes including the VHL, NF1, RET, SDHD, SDHB, SDHA, MAX, and TMEM127 genes.
More than half of the children and adolescents diagnosed with pheochromocytoma or paraganglioma have an inherited syndrome or gene change that increased the risk of cancer. Genetic counseling (a discussion with a trained professional about inherited diseases) and testing is an important part of the treatment plan.
Some tumors do not make extra adrenaline or noradrenaline and do not cause symptoms. These tumors may be found when a lump forms in the neck or when a test or procedure is done for another reason. Signs and symptoms of pheochromocytoma and paraganglioma occur when too much adrenaline or noradrenaline is released into the blood. These and other symptoms may be caused by pheochromocytoma, paraganglioma, or other conditions. Check with your child’s doctor if your child has any of the following:
- High blood pressure.
- Headache.
- Heavy sweating for no known reason.
- A strong, fast, or irregular heartbeat.
- Feeling shaky.
- Being extremely pale.
- Dizziness.
- Being irritable or nervous.
These signs and symptoms may come and go but high blood pressure is more likely to occur for long periods of time in young patients. These signs and symptoms may also occur with physical activity, injury, anesthesia, surgery to remove the tumor, eating foods such as chocolate and cheese, or while passing urine (if the tumor is in the bladder).
Tests used to diagnose and stage pheochromocytoma and paraganglioma depend on the signs and symptoms and the patient’s family history. They may include:
- Physical exam and history.
- PET scan.
- CT scan (CAT scan).
- MRI (magnetic resonance imaging).
See the General Information section for a description of these tests and procedures.
Other tests and procedures used to diagnose pheochromocytoma and paraganglioma include the following:
- Plasma-free metanephrines test: A blood test that measures the amount of metanephrines in the blood. Metanephrines are substances that are made when the body breaks down adrenaline or noradrenaline. Pheochromocytomas and paragangliomas can make large amounts of adrenaline and noradrenaline and cause high levels of metanephrines in both the blood and urine.
- Blood catecholamine studies: A procedure in which a blood sample is checked to measure the amount of certain catecholamines (adrenaline or noradrenaline) released into the blood. Substances caused by the breakdown of these catecholamines are also measured. An unusual (higher- or lower-than-normal) amount of a substance can be a sign of disease in the organ or tissue that makes it. Higher-than-normal amounts may be a sign of pheochromocytoma or paraganglioma.
- Twenty-four-hour urine test: A test in which urine is collected for 24 hours to measure the amounts of catecholamines (adrenaline or noradrenaline) or metanephrines in the urine. Substances caused by the breakdown of these catecholamines are also measured. An unusual (higher- or lower-than-normal) amount of a substance can be a sign of disease in the organ or tissue that makes it. Higher-than-normal amounts may be a sign of pheochromocytoma or paraganglioma.
- MIBG scan: A procedure used to find neuroendocrine tumors, such as pheochromocytoma and paraganglioma. A very small amount of a substance called radioactive MIBG is injected into a vein and travels through the bloodstream. Neuroendocrine tumor cells take up the radioactive MIBG and are detected by a scanner. Scans may be taken over 1-3 days. An iodine solution may be given before or during the test to keep the thyroid gland from absorbing too much of the MIBG.
- Somatostatin receptor scintigraphy: A type of radionuclide scan that may be used to find tumors. A very small amount of radioactive octreotide (a hormone that attaches to tumors) is injected into a vein and travels through the blood. The radioactive octreotide attaches to the tumor and a special camera that detects radioactivity is used to show where the tumors are in the body. This procedure is also called octreotide scan and SRS.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of pheochromocytoma and paraganglioma in children may include the following:
- Surgery to completely remove the tumor.
- Combination chemotherapy, high-dose 131I-MIBG, and targeted therapy for tumors that have spread.
Before surgery, drug therapy with alpha-blockers to control blood pressure and beta-blockers to control heart rate are given. If both adrenal glands are removed, life-long hormone therapy to replace hormones made by the adrenal glands is needed after surgery.
Treatment of recurrent pheochromocytoma and paraganglioma in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
Skin Cancer (Melanoma, Squamous Cell Cancer, Basal Cell Cancer)
Skin cancer is a disease in which malignant (cancer) cells form in the tissues of the skin. The skin is the body’s largest organ. It protects against heat, sunlight, injury, and infection. Skin also helps control body temperature and stores water, fat, and vitamin D. The skin has several layers, but the two main layers are the epidermis (upper or outer layer) and the dermis (lower or inner layer). Skin cancer begins in the epidermis, which is made up of three kinds of cells:
- Melanocytes: Found in the lower part of the epidermis, these cells make melanin, the pigment that gives skin its natural color. When skin is exposed to the sun, melanocytes make more pigment and cause the skin to darken.
- Squamous cells: Thin, flat cells that form the top layer of the epidermis.
- Basal cells: Round cells under the squamous cells.
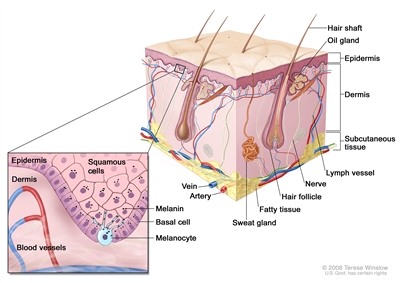
Anatomy of the skin, showing the epidermis, dermis, and subcutaneous tissue. Melanocytes are in the layer of basal cells at the deepest part of the epidermis.
There are three types of skin cancer:
- Melanoma.
- Squamous cell skin cancer.
- Basal cell skin cancer.
Melanoma
Even though melanoma is rare, it is the most common skin cancer in children. It occurs more often in adolescents aged 15 to 19 years.
The risk of having melanoma is increased by having the following conditions:
- Giant melanocytic nevi (large black spots, which may cover the trunk and thigh).
- Xeroderma pigmentosum.
- Multiple endocrine neoplasia type I (MEN1) syndrome (Werner syndrome).
- Hereditary retinoblastoma.
- Having a weakened immune system.
Other risk factors for melanoma in all age groups include:
- Having a fair complexion, which includes the following:
- Fair skin that freckles and burns easily, does not tan, or tans poorly.
- Blue or green or other light-colored eyes.
- Red or blond hair.
- Being exposed to natural sunlight or artificial sunlight (such as from tanning beds) over long periods of time.
- Having several large or many small moles.
- Having a family history or personal history of unusual moles (atypical nevus syndrome).
- Having a family history of melanoma.
Signs and symptoms of melanoma include the following:
- A mole that:
- changes in size, shape, or color.
- has irregular edges or borders.
- is more than one color.
- is asymmetrical (if the mole is divided in half, the 2 halves are different in size or shape).
- itches.
- oozes, bleeds, or is ulcerated (a hole forms in the skin when the top layer of cells breaks down and the tissue below shows through).
- Change in pigmented (colored) skin.
- Satellite moles (new moles that grow near an existing mole).
Tests to diagnose and stage melanoma may include the following:
- Physical exam and history.
- X-ray of the chest.
- CT scan.
- MRI.
- PET scan.
See the General Information section for a description of these tests and procedures.
Other tests and procedures used to diagnose melanoma include the following:
- Skin exam: A doctor or nurse checks the skin for bumps or spots that look abnormal in color, size, shape, or texture.
- Biopsy: All or part of the abnormal-looking growth is cut from the skin and viewed under a microscope by a pathologist to check for cancer cells. There are four main types of skin biopsies:
- Shave biopsy: A sterile razor blade is used to “shave off” the abnormal-looking growth.
- Punch biopsy: A special instrument called a punch or a trephine is used to remove a circle of tissue from the abnormal-looking growth.
- Excisional biopsy: A scalpel is used to remove the entire growth.
- Wide local excision: A scalpel is used to remove the growth and some of the normal tissue around the area, to check for cancer cells. Skin grafting may be needed to cover the area where tissue was removed.
- Sentinel lymph node biopsy: The removal of the sentinel lymph node during surgery. The sentinel lymph node is the first lymph node to receive lymphatic drainage from a tumor. It is the first lymph node the cancer is likely to spread to from the tumor. A radioactive substance and/or blue dye is injected near the tumor. The substance or dye flows through the lymph ducts to the lymph nodes. The first lymph node to receive the substance or dye is removed. A pathologist views the tissue under a microscope to look for cancer cells. If cancer cells are not found, it may not be necessary to remove more lymph nodes.
- Lymph node dissection: A surgical procedure in which lymph nodes are removed and a sample of tissue is checked under a microscope for signs of cancer. For a regional lymph node dissection, some of the lymph nodes in the tumor area are removed. For a radical lymph node dissection, most or all of the lymph nodes in the tumor area are removed. This procedure is also called a lymphadenectomy.
Treatment of Melanoma
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of melanoma is surgery to remove the tumor and some tissue around the tumor.
If cancer has spread to nearby lymph nodes, treatment is surgery to remove the lymph nodes with cancer. Immunotherapy with high-dose interferon or ipilimumab may also be given.
Treatment of melanoma that has spread beyond the lymph nodes may include the following:
- Immunotherapy (ipilimumab).
- A clinical trial of a new targeted therapy drug.
Treatment of recurrent melanoma in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
- A clinical trial of a new targeted therapy or immunotherapy drug.
See the PDQ summary on adult Melanoma Treatment for more information.
Squamous Cell and Basal Cell Skin Cancer
Nonmelanoma skin cancers (squamous cell and basal cell cancers) are very rare in children and adolescents. The risk of squamous cell or basal cell cancer is increased by the following:
- Being exposed to natural sunlight or artificial sunlight (such as from tanning beds) over long periods of time.
- Having a fair complexion, which includes the following:
- Fair skin that freckles and burns easily, does not tan, or tans poorly.
- Blue or green or other light-colored eyes.
- Red or blond hair.
- Having actinic keratosis.
- Past treatment with radiation.
- Having a weakened immune system.
Signs of squamous cell and basal cell skin cancer include the following:
- A sore that does not heal.
- Areas of the skin that are:
- Small, raised, smooth, shiny, and waxy.
- Small, raised, and red or reddish-brown.
- Flat, rough, red or brown, and scaly.
- Scaly, bleeding, or crusty.
- Similar to a scar and firm.
Tests to diagnose squamous cell and basal cell skin cancer include the following:
- Skin exam: A doctor or nurse checks the skin for bumps or spots that look abnormal in color, size, shape, or texture.
- Biopsy: All or part of a growth that doesn’t look normal is cut from the skin and viewed under a microscope by a pathologist to check for signs of cancer. There are three main types of skin biopsies:
- Shave biopsy: A sterile razor blade is used to “shave off” the growth that does not look normal.
- Punch biopsy: A special instrument called a punch or a trephine is used to remove a circle of tissue from the growth that does not look normal.
- Excisional biopsy: A scalpel is used to remove the entire growth.
Treatment of Squamous Cell and Basal Cell Skin Cancer
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of squamous cell and basal cell cancer in children may include the following:
- Surgery to remove the tumor. This may include Mohs micrographic surgery.
Mohs micrographic surgery is a type of surgery used for skin cancers. The tumor is cut from the skin in thin layers. During surgery, the edges of the tumor and each layer of tumor removed are viewed through a microscope to check for cancer cells. Layers continue to be removed until no more cancer cells are seen. This type of surgery removes as little normal tissue as possible and is often used to remove skin cancer on the face.
Treatment of recurrent squamous cell and basal cell cancer in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
See the PDQ summary on adult Skin Cancer Treatment for more information.
Intraocular (Uveal) Melanoma
Intraocular melanoma begins in the middle of three layers of the wall of the eye. The outer layer includes the white sclera (the “white of the eye”) and the clear cornea at the front of the eye. The inner layer has a lining of nerve tissue, called the retina, which senses light and sends images along the optic nerve to the brain. The middle layer, where intraocular melanoma forms, is called the uvea or uveal tract, and has three main parts: the iris, the ciliary body, and the choroid.
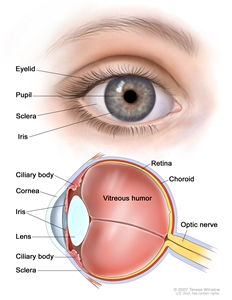
Anatomy of the eye, showing the outside and inside of the eye including the sclera, cornea, iris, ciliary body, choroid, retina, vitreous humor, and optic nerve. The vitreous humor is a liquid that fills the center of the eye.
Risk Factors
The risk of intraocular melanoma is increased by any of the following:
- Light eye color.
- Fair skin color.
- Not being able to tan.
- Oculodermal melanocytosis.
- Presence of cutaneous nevi.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of intraocular melanoma in children is similar to treatment for adults and may include the following:
- Surgery to remove the tumor.
- Laser surgery.
- Radiation therapy.
Treatment of recurrent intraocular melanoma in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
See the PDQ summary on adult Intraocular (Uveal) Melanoma Treatment for more information.
Chordoma
Chordoma is a very rare type of bone tumor that forms anywhere along the spine from the base of the skull to the tailbone. In children and adolescents, chordomas develop more often in the base of the skull, making them hard to remove completely with surgery.
Childhood chordoma is linked to the condition tuberous sclerosis, a genetic disorder in which tumors that are benign (not cancer) form in the kidneys, brain, eyes, heart, lungs, and skin.
Signs and Symptoms
Chordoma may cause any of the following signs and symptoms. Check with your child’s doctor if your child has any of the following:
- Headache.
- Neck or back pain.
- Double vision.
- Paralysis of the muscles in the face.
- Numbness, tingling, or weakness of the arms and legs.
- A change in bowel or bladder habits.
Other conditions that are not chordoma may cause these same signs and symptoms.
Chordomas may recur (come back), usually in the same place, but sometimes they recur in other areas of bone or in the lungs.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of chordoma in children may include the following:
- Surgery to remove as much of the tumor as possible, followed by radiation therapy. Proton beam radiation therapy may be used.
Treatment of recurrent chordoma in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change. Patients with changes in the SMARCB1 gene may be treated with tazemetostat in this clinical trial.
Cancer of Unknown Primary Site
Carcinoma of unknown primary is a rare disease in which malignant (cancer) cells are found in the body but the place the cancer began is not known. Cancer can form in any tissue of the body. The primary cancer (the cancer that first formed) can spread to other parts of the body. This process is called metastasis. Cancer cells usually look like the cells in the type of tissue in which the cancer began. For example, breast cancer cells may spread to the lung. Because the cancer began in the breast, the cancer cells in the lung look like breast cancer cells.
Sometimes doctors find where the cancer has spread but cannot find where in the body the cancer first began to grow. This type of cancer is called a cancer of unknown primary or occult primary tumor.
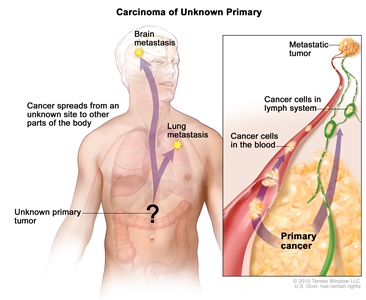
In carcinoma of unknown primary, cancer cells have spread in the body but the place where the primary cancer began is unknown.
Tests are done to find where the primary cancer began and to get information about where the cancer has spread. When tests are able to find the primary cancer, the cancer is no longer a cancer of unknown primary and treatment is based on the type of primary cancer.
Because the place where the cancer started is not known, many different tests and procedures may be needed to find out what type of cancer it is. If tests show there may be cancer, a biopsy is done. A biopsy is the removal of cells or tissues so they can be viewed under a microscope by a pathologist. The pathologist views the tissue to look for cancer cells and to find out the type of cancer. The type of biopsy that is done depends on the part of the body being tested for cancer. One of the following types of biopsies may be used:
- Fine-needle aspiration (FNA) biopsy: The removal tissue or fluid using a thin needle.
- Core biopsy: The removal of tissue using a wide needle.
- Incisional biopsy: The removal of part of a lump or a sample of tissue.
- Excisional biopsy: The removal of an entire lump of tissue.
When the type of cancer cells or tissue removed is different from the type of cancer cells expected to be found, a diagnosis of cancer of unknown primary may be made. The cells in the body have a certain look that depends on the type of tissue they come from. For example, a sample of cancer tissue taken from the breast is expected to be made up of breast cells. However, if the sample of tissue is a different type of cell (not made up of breast cells), it is likely that the cells have spread to the breast from another part of the body.
Adenocarcinomas, melanomas, and embryonal tumors are common tumor types that appear and it is not known where the cancer first formed. Embryonal tumors such as rhabdomyosarcomas and neuroblastomas are most common in children.
Treatment
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment depends on what the cancer cells look like under a microscope, the patient’s age, signs and symptoms, and where the cancer has spread in the body. Treatment is usually the following:
- Chemotherapy.
- Targeted therapy.
- Radiation therapy.
Treatment of recurrent cancer of unknown primary in children may include the following:
- A clinical trial that checks a sample of the patient’s tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
See the PDQ summary on adult Carcinoma of Unknown Primary for more information.
To Learn More About Childhood Cancer
For more information from the National Cancer Institute about unusual cancers of childhood, see the following:
- Genetic Testing for Inherited Cancer Susceptibility Syndromes
- Computed Tomography (CT) Scans and Cancer
- MyPART – My Pediatric and Adult Rare Tumor Network
For more childhood cancer information and other general cancer resources, see the following:
- About Cancer
- Childhood Cancers
- CureSearch for Children’s Cancer
- Late Effects of Treatment for Childhood Cancer
- Adolescents and Young Adults with Cancer
- Children with Cancer: A Guide for Parents
- Cancer in Children and Adolescents
- Staging
- Coping with Cancer
- Questions to Ask Your Doctor about Cancer
- For Survivors and Caregivers
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute’s (NCI’s) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government’s center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of unusual cancers of childhood. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary (“Updated”) is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Pediatric Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become “standard.” Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI’s website. For more information, call the Cancer Information Service (CIS), NCI’s contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary].”
The best way to cite this PDQ summary is:
PDQ® Pediatric Treatment Editorial Board. PDQ Unusual Cancers of Childhood Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/childhood-cancers/patient/unusual-cancers-childhood-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389276]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s E-mail Us.
Last Revised: 2019-07-01
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI’s Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.
Topic Contents
- General Information About Unusual Cancers of Childhood
- Treatment Option Overview
- Unusual Cancers of the Head and Neck
- Unusual Cancers of the Chest
- Unusual Cancers of the Abdomen
- Unusual Cancers of the Reproductive and Urinary Systems
- Other Rare Unusual Cancers of Childhood
- To Learn More About Childhood Cancer
- About This PDQ Summary
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.

