Top of the pageCheck Your Symptoms
Abdominal Pain, Age 12 and Older
Topic Overview
The cause of abdominal problems can be hard to pinpoint. Sometimes minor and serious abdominal problems start with the same symptoms. Fortunately, most abdominal problems are minor, and home treatment is all that is needed.
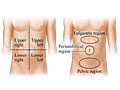
Many times the exact cause of abdominal pain is hard to find. The severity of your pain, its location, and other symptoms you have may help determine what is causing the pain.
- Generalized pain occurs in half of the abdomen or more. Generalized pain can occur with many different illnesses and will usually go away without medical treatment. Indigestion and an upset stomach are common problems that can cause generalized pain. Home treatment may help relieve some of the discomfort. Generalized mild pain or crampy pain that becomes more severe over several hours may be a symptom of a blockage of the intestines (bowel obstruction).
- Localized pain is located in one area of the abdomen. Localized pain that comes on suddenly and gets worse is more likely to be a symptom of a serious problem. The pain of appendicitis may start as generalized pain, but it often moves (localizes) to one area of the abdomen. The pain from gallbladder disease or peptic ulcer disease often starts in one area of the abdomen and stays in that same location. Localized pain that gradually becomes more severe may be a symptom of inflammation of an abdominal organ.
- Cramping is a type of pain that comes and goes (intermittent) or that changes in position or severity. Cramping is rarely serious if it is relieved by passing gas or a stool. Many women have cramping pain with their menstrual periods. Generalized cramping pain is usually not a cause for concern unless it gets worse, lasts for longer than 24 hours, or localizes. Cramping that starts suddenly with diarrhea or other minor health problems can be quite painful but is usually not serious.
Occasionally, severe pain that comes on suddenly may be a symptom of a rupture of the stomach or intestines (perforation), torsion of the testicle or ovary, a kidney stone, gallbladder disease, or blood vessel problems, such as an aortic aneurysm. The pain caused by appendicitis or gallbladder disease may increase when you move or cough. Pain that increases with movement or coughing and does not appear to be caused by strained muscles is more likely to be a symptom of a serious problem. A visit to a doctor is usually needed when severe abdominal pain comes on suddenly, or when new and different mild pain slowly becomes more severe over several hours or days.
After a minor abdominal injury, pain, nausea, or vomiting may occur but often gets better in a few minutes. Pain and other symptoms that continue, increase, or develop following an injury may mean an abdominal organ has been damaged.
Many medicines can cause abdominal pain. Some medicines also cause side effects, such as constipation, that can make abdominal pain worse.
Abdominal symptoms can also occur from an infection passed on by animals or while traveling to a foreign country.
Specific abdominal symptoms have been linked to ovarian cancer. These symptoms include abdominal or pelvic pain, increased abdominal size or bloating, and trouble eating or feeling full quickly. If you have one or more of these symptoms, and it occurs almost daily for more than 2 or 3 weeks, talk with your doctor.
Check your symptoms to decide if and when you should see a doctor.
Check Your Symptoms
The medical assessment of symptoms is based on the body parts you have.
- If you are transgender or nonbinary, choose the sex that matches the body parts (such as ovaries, testes, prostate, breasts, penis, or vagina) you now have in the area where you are having symptoms.
- If your symptoms aren’t related to those organs, you can choose the gender you identify with.
- If you have some organs of both sexes, you may need to go through this triage tool twice (once as “male” and once as “female”). This will make sure that the tool asks the right questions for you.
Many things can affect how your body responds to a symptom and what kind of care you may need. These include:
- Your age. Babies and older adults tend to get sicker quicker.
- Your overall health. If you have a condition such as diabetes, HIV, cancer, or heart disease, you may need to pay closer attention to certain symptoms and seek care sooner.
- Medicines you take. Certain medicines, herbal remedies, and supplements can cause symptoms or make them worse.
- Recent health events, such as surgery or injury. These kinds of events can cause symptoms afterwards or make them more serious.
- Your health habits and lifestyle, such as eating and exercise habits, smoking, alcohol or drug use, sexual history, and travel.
Try Home Treatment
You have answered all the questions. Based on your answers, you may be able to take care of this problem at home.
- Try home treatment to relieve the symptoms.
- Call your doctor if symptoms get worse or you have any concerns (for example, if symptoms are not getting better as you would expect). You may need care sooner.
With cramping pain in the belly:
- The pain may hurt a little or a lot.
- The amount of pain may change from minute to minute. Cramps often get better when you pass gas or have a bowel movement.
- The pain may feel like a tightness or pinching in your belly.
- The pain may be in one specific area or be over a larger area. It may move around.
Shock is a life-threatening condition that may quickly occur after a sudden illness or injury.
Adults and older children often have several symptoms of shock. These include:
- Passing out (losing consciousness).
- Feeling very dizzy or lightheaded, like you may pass out.
- Feeling very weak or having trouble standing.
- Not feeling alert or able to think clearly. You may be confused, restless, fearful, or unable to respond to questions.
If you’re not sure if a fever is high, moderate, or mild, think about these issues:
With a high fever:
- You feel very hot.
- It is likely one of the highest fevers you’ve ever had. High fevers are not that common, especially in adults.
With a moderate fever:
- You feel warm or hot.
- You know you have a fever.
With a mild fever:
- You may feel a little warm.
- You think you might have a fever, but you’re not sure.
Temperature varies a little depending on how you measure it. For adults and children age 12 and older, these are the ranges for high, moderate, and mild, according to how you took the temperature.
Oral (by mouth) temperature
- High: 104°F (40°C) and higher
- Moderate: 100.4°F (38°C) to 103.9°F (39.9°C)
- Mild: 100.3°F (37.9°C) and lower
A forehead (temporal) scanner is usually 0.5°F (0.3°C) to 1°F (0.6°C) lower than an oral temperature.
Ear or rectal temperature
- High: 105°F (40.6°C) and higher
- Moderate: 101.4°F (38.6°C) to 104.9°F (40.5°C)
- Mild: 101.3°F (38.5°C) and lower
Armpit (axillary) temperature
- High: 103°F (39.5°C) and higher
- Moderate: 99.4°F (37.4°C) to 102.9°F (39.4°C)
- Mild: 99.3°F (37.3°C) and lower
Certain health conditions and medicines weaken the immune system’s ability to fight off infection and illness. Some examples in adults are:
- Diseases such as diabetes, cancer, heart disease, and HIV/AIDS.
- Long-term alcohol and drug problems.
- Steroid medicines, which may be used to treat a variety of conditions.
- Chemotherapy and radiation therapy for cancer.
- Other medicines used to treat autoimmune disease.
- Medicines taken after organ transplant.
- Not having a spleen.
Pain in adults and older children
- Severe pain (8 to 10): The pain is so bad that you can’t stand it for more than a few hours, can’t sleep, and can’t do anything else except focus on the pain.
- Moderate pain (5 to 7): The pain is bad enough to disrupt your normal activities and your sleep, but you can tolerate it for hours or days. Moderate can also mean pain that comes and goes even if it’s severe when it’s there.
- Mild pain (1 to 4): You notice the pain, but it is not bad enough to disrupt your sleep or activities.
It is easy for your diabetes to become out of control when you are sick. Because of an illness:
- Your blood sugar may be too high or too low.
- You may not be able take your diabetes medicine (if you are vomiting or having trouble keeping food or fluids down).
- You may not know how to adjust the timing or dose of your diabetes medicine.
- You may not be eating enough or drinking enough fluids.
An illness plan for people with diabetes usually covers things like:
- How often to test blood sugar and what the target range is.
- Whether and how to adjust the dose and timing of insulin or other diabetes medicines.
- What to do if you have trouble keeping food or fluids down.
- When to call your doctor.
The plan is designed to help keep your diabetes in control even though you are sick. When you have diabetes, even a minor illness can cause problems.
You can get dehydrated when you lose a lot of fluids because of problems like vomiting or fever.
Symptoms of dehydration can range from mild to severe. For example:
- You may feel tired and edgy (mild dehydration), or you may feel weak, not alert, and not able to think clearly (severe dehydration).
- You may pass less urine than usual (mild dehydration), or you may not be passing urine at all (severe dehydration).
Severe dehydration means:
- Your mouth and eyes may be extremely dry.
- You may pass little or no urine for 12 or more hours.
- You may not feel alert or be able to think clearly.
- You may be too weak or dizzy to stand.
- You may pass out.
Moderate dehydration means:
- You may be a lot more thirsty than usual.
- Your mouth and eyes may be drier than usual.
- You may pass little or no urine for 8 or more hours.
- You may feel dizzy when you stand or sit up.
Mild dehydration means:
- You may be more thirsty than usual.
- You may pass less urine than usual.
Blood in the stool can come from anywhere in the digestive tract, such as the stomach or intestines. Depending on where the blood is coming from and how fast it is moving, it may be bright red, reddish brown, or black like tar.
A little bit of bright red blood on the stool or on the toilet paper is often caused by mild irritation of the rectum. For example, this can happen if you have to strain hard to pass a stool or if you have a hemorrhoid.
Certain medicines and foods can affect the color of stool. Diarrhea medicines (such as Pepto-Bismol) and iron tablets can make the stool black. Eating lots of beets may turn the stool red. Eating foods with black or dark blue food coloring can turn the stool black.
If you take aspirin or some other medicine (called a blood thinner) that prevents blood clots, it can cause some blood in your stools. If you take a blood thinner and have ongoing blood in your stools, call your doctor to discuss your symptoms.
Symptoms of a heart attack may include:
- Chest pain or pressure, or a strange feeling in the chest.
- Sweating.
- Shortness of breath.
- Nausea or vomiting.
- Pain, pressure, or a strange feeling in the back, neck, jaw, or upper belly, or in one or both shoulders or arms.
- Lightheadedness or sudden weakness.
- A fast or irregular heartbeat.
The more of these symptoms you have, the more likely it is that you’re having a heart attack. Chest pain or pressure is the most common symptom, but some people, especially women, may not notice it as much as other symptoms. You may not have chest pain at all but instead have shortness of breath, nausea, or a strange feeling in your chest or other areas.
Many prescription and nonprescription medicines can cause belly pain or cramping. A few examples are:
- Aspirin, ibuprofen (such as Advil or Motrin), and naproxen (such as Aleve).
- Antibiotics.
- Antidiarrheals.
- Laxatives.
- Iron supplements.
Call 911 Now
Based on your answers, you need emergency care.
Call911or other emergency services now.
Seek Care Now
Based on your answers, you may need care right away. The problem is likely to get worse without medical care.
- Call your doctor now to discuss the symptoms and arrange for care.
- If you cannot reach your doctor or you don’t have one, seek care in the next hour.
- You do not need to call an ambulance unless:
- You cannot travel safely either by driving yourself or by having someone else drive you.
- You are in an area where heavy traffic or other problems may slow you down.
Seek Care Today
Based on your answers, you may need care soon. The problem probably will not get better without medical care.
- Call your doctor today to discuss the symptoms and arrange for care.
- If you cannot reach your doctor or you don’t have one, seek care today.
- If it is evening, watch the symptoms and seek care in the morning.
- If the symptoms get worse, seek care sooner.
Make an Appointment
Based on your answers, the problem may not improve without medical care.
- Make an appointment to see your doctor in the next 1 to 2 weeks.
- If appropriate, try home treatment while you are waiting for the appointment.
- If symptoms get worse or you have any concerns, call your doctor. You may need care sooner.
Call 911 Now
Based on your answers, you need emergency care.
Call911or other emergency services now.
After you call 911 , the operator may tell you to chew 1 adult-strength (325 mg) or 2 to 4 low-dose (81 mg) aspirin. Wait for an ambulance. Do not try to drive yourself.
Home Treatment
Most of the time, abdominal pain improves with home treatment and you do not need a visit to a doctor. Specific home treatment for abdominal pain often depends on the symptoms you have along with the pain, such as diarrhea or nausea and vomiting.
If you have mild abdominal pain without other symptoms, try the following:
- Rest until you are feeling better.
- Drink plenty of fluids to prevent dehydration. You may find that taking small, frequent sips of a beverage is easier on your stomach than trying to drink a whole glass at once. Do not drink carbonated or caffeinated drinks, such as soda pop, tea, or coffee.
- Try eating several small meals instead of 2 or 3 large ones. Eat mild foods, such as rice, dry toast or crackers, bananas, and applesauce. Do not eat spicy foods, other fruits, alcohol, and drinks that have caffeine until 48 hours after all symptoms have gone away.
- Do not eat foods that are high in fat. Foods high in fat may increase your abdominal pain.
- Do not use aspirin or other nonsteroidal anti-inflammatory medicines, such as ibuprofen and naproxen. These medicines may irritate your stomach and increase your pain.
Symptoms to watch for during home treatment
Call your doctor if any of the following occur during home treatment:
- Pain increases, does not improve, or localizes to one specific area of the abdomen.
- Other symptoms develop, such as diarrhea, nausea, vomiting, or a fever.
- Symptoms become more severe or frequent.
Prevention
Abdominal pain can often be prevented.
- Develop regular bowel habits to prevent abdominal pain caused by constipation. For more information, see the topic Constipation, Age 12 and Older.
- Develop regular eating habits. Overeating is a common cause of abdominal discomfort. Eat slowly and stop when you feel full.
- To prevent abdominal pain caused by swallowing air (aerophagia), do not chew gum or drink carbonated beverages.
- Prevent abdominal injuries by wearing your seat belt safely and correctly every time you drive or are a passenger in a car.
- Wear both your lap and shoulder belts. The shoulder strap should cross the collarbone, and the lap belt should fit low and tight.
- Do not wear your shoulder strap slipped behind the back or under the arm. This dangerous habit can cause severe injury, especially in cars with air bags.
Preparing For Your Appointment
To prepare for your appointment, see the topicMaking the Most of Your Appointment.
You can help your doctor diagnose and treat your condition by being prepared to answer the following questions:
- How long have you had the pain?
- What were you doing when the pain started?
- Did the pain start suddenly or develop gradually?
- How severe is your pain? Rate your pain on a scale of 1 to 10.
- Is your pain generalized or localized? If you have localized pain, where is it located?
- Is your pain cramping, a steady ache, burning, or a tearing sensation?
- Is your pain changing? If so, how?
- Is the pain constant, or does it come and go?
- Have you had other symptoms, such as nausea, vomiting, constipation, diarrhea, a change in urination, or fever?
- Have you had this type of pain before? If so, did you see a doctor? How was the pain treated?
- What makes the pain better? What makes the pain worse?
- Have you recently traveled outside of the country?
- Have you drunk any untreated well, stream, or lake water?
- Do you have any health risks?
Current as of: June 26, 2019
Author: Healthwise Staff
Medical Review:William H. Blahd Jr. MD, FACEP – Emergency Medicine & Adam Husney MD – Family Medicine & Kathleen Romito MD – Family Medicine
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.