Cervical Disc Herniation
Topic Overview
What is cervical disc herniation?
The bones (vertebrae) that form the spine in your back are cushioned by round, flat discs. When these discs are healthy, they act as shock absorbers for the spine and keep the spine flexible. If they become damaged, they may bulge abnormally or break open (rupture), in what is called a herniated or slipped disc. Herniated discs can occur in any part of the spine, but they are most common in the neck (cervical) and lower back (lumbar) spine. The seven vertebrae between the head and the chest make up the cervical spine.
What causes cervical disc herniation?
A herniated disc usually is caused by wear and tear of the disc (also called disc degeneration). As we age, our discs lose some of the fluid that helps them stay flexible. A herniated disc also may result from injuries to the spine, which may cause tiny tears or cracks in the outer layer (annulus or capsule) of the disc. The jellylike material (nucleus) inside the disc may be forced out through the tears or cracks in the capsule, which causes the disc to bulge, break open (rupture), or break into fragments.
Herniated discs are much more common in people who smoke.
What are the symptoms?
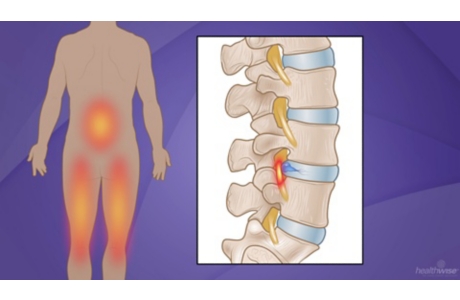
Herniated discs in the neck (cervical spine) can cause pain, numbness, or weakness in the neck, shoulders, chest, arms, and hands. In some cases a very large herniated disc in the neck may cause weakness or unusual tingling affecting other parts of the body, including the legs.
How is cervical disc herniation diagnosed?
A doctor usually can diagnose a herniated disc from your history of symptoms and a physical exam. Your doctor will ask about pain and numbness that might be caused by irritation of one or more of the nerves in the cervical spine. If your symptoms suggest a cervical herniated disc, rest and rehabilitation (rehab) often are recommended before further testing is done. If other conditions are suspected, or if there is no improvement in symptoms after a period of rest and rehab, imaging tests such as X-ray, magnetic resonance imaging (MRI), or computerized tomography (CT scan) may be done.
How is it treated?
In most cases, cervical herniated discs are first treated with nonsurgical treatment, including rest or modified activities, medicines to relieve pain and inflammation, and exercises, as recommended by your doctor. Your doctor may recommend that you see a physical therapist to learn how to do exercises and protect your neck, and perhaps for other treatment such as traction. Traction is gentle, steady pulling on the head to stretch the neck and allow the small joints between the neck bones to spread a little. If symptoms continue, your doctor may try stronger medicine such as corticosteroids. Symptoms usually improve over time. But if the herniated disc is squeezing your spinal cord or nerves and/or you are having weakness, constant pain, or decreased control of your bladder or bowels, surgery will be considered. In rare cases, an artificial disc may be used to replace the disc that is removed.
References
Other Works Consulted
- American Academy of Orthopaedic Surgeons and American Academy of Pediatrics (2010). Cervical radiculopathy. In JF Sarwark, ed., Essentials of Musculoskeletal Care, 4th ed., pp. 922–924. Rosemont, IL: American Academy of Orthopaedic Surgeons.
- Mostoufi A (2015). Cervical radiculopathy. In WR Frontera et al., eds., Essentials of Physical Medicine and Rehabilitation, 3rd ed., pp. 22–30. Philadelphia: Saunders.
- North American Spine Society (2010). Diagnosis and treatment of cervical radiculopathy from degenerative disorders: Evidence-based clinical guidelines for multidisciplinary spine care. Available online: http://www.spine.org/Documents/Cervical_Radiculopathy.pdf.
- Sasso RC, et al. (2011). Results of cervical arthroplasty compared with anterior discectomy and fusion: Four-year clinical outcomes in a prospective, randomized controlled trial. Journal of Bone and Joint Surgery, 93(18 ): 1684–1692.
Current as of: June 26, 2019
Author: Healthwise Staff
Medical Review:William H. Blahd Jr. MD, FACEP – Emergency Medicine & E. Gregory Thompson MD – Internal Medicine & Adam Husney MD – Family Medicine & Kathleen Romito MD – Family Medicine
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.