Cleft Palate
Topic Overview
What is cleft palate?
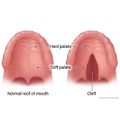
Cleft palate is a treatable birth defect. It happens when the roof of the baby’s mouth (palate) doesn’t develop normally during pregnancy, leaving an opening (cleft) in the palate that may go through to the nasal cavity. A cleft can form on any part of the palate, including the front part of the roof of the mouth (hard palate) or the small flap of tissue that hangs down from the soft palate (uvula). It may appear by itself or along with other birth defects of the face and skull, such as a cleft lip.
Cleft palate and cleft lip are the most common birth defects of the head and neck. Until a cleft palate is treated with surgery, it can cause problems with feeding, speech, and hearing.
What causes cleft palate?
Doctors aren’t sure what causes it. But your baby may be more likely to have a cleft palate if you:
- Use certain medicines while you’re pregnant.
- Use alcohol or illegal drugs while you’re pregnant.
- Smoke while you’re pregnant.
- Are exposed to radiation or infections while you’re pregnant.
- Have a family history of cleft palate.
It’s important to take good care of yourself before and during your pregnancy so that your baby will be as healthy as possible.
If someone in your family was born with a cleft palate, you may want to think about genetic counseling. It can help you understand your chances of having a child with a cleft palate.
What are the symptoms?
Some forms of cleft palate are easy to see when the child is born. But even if the cleft palate doesn’t affect how the baby’s face looks, it can usually be seen inside the mouth.
The location of the cleft matters more than how it looks. A small cleft in the soft palate may cause more problems—because of its effect on speech—than a large cleft that is easy to see.
A baby with a cleft palate often has feeding problems, because he or she isn’t able to suck and swallow normally. But this doesn’t always last, especially with treatment.
How is a cleft palate diagnosed?
A doctor can diagnose a cleft palate by doing a physical exam of the baby’s mouth shortly after birth.
Fetal ultrasound can sometimes find cleft palate as early as 14 to 16 weeks into pregnancy, especially if the cleft palate is severe and occurs along with a cleft lip. But ultrasound doesn’t always find the problem, so doctors can’t always rely on it to diagnose a cleft palate.
How is it treated?
Treatment involves a team of health care providers. The type of treatment depends on how severe the problem is.
Surgery is the most common treatment for a cleft palate. For the most part, it’s done before a child is 12 months old.footnote 1 Before surgery, your baby may need treatment for breathing or feeding problems. He or she may also wear a mouth support (such as a dental splint) or a soft dental molding insert along with medical adhesive tape.
As your child grows, he or she will probably need more than one operation. But the problem is normally fixed by the time a child is a teen. Although surgery often leaves scars, the palate usually heals well and leaves few signs of the cleft. A child’s facial bones most often grow normally, and the child speaks more clearly.
Some children who have a cleft palate need more treatment for other problems, such as speech, hearing, or teeth problems; sinus and ear infections; and problems from surgery.
What can you do at home to help your child and yourself?
If your baby is born with a cleft palate, get help with feeding. A nurse can guide you on feeding techniques. Watch for infections and hearing or teeth problems too.
As your child grows, pay special attention to dental care, hearing, and speech. You can also support your child’s self-esteem. Explain how a cleft palate forms and how having one has been a part of making your child strong.
Caring for a child who has a cleft palate can take a lot of time and patience. Seek support from friends and family. You can join a support group to meet others who are going through similar challenges.
References
Citations
- Heike CL, Cunningham ML (2011). Craniofacial disorders. In CD Rudolph et al., eds., Rudolph’s Pediatrics, 22nd ed., pp. 705–713. New York: McGraw-Hill.
Other Works Consulted
- American College of Obstetricians and Gynecologists (2003, reaffirmed 2011). Neural tube defects. ACOG Practice Bulletin No. 44. Obstetrics and Gynecology, 102(1): 203–210.
- Bessell A, et al. (2011). Feeding interventions for growth and development in infants with cleft lip. Cochrane Database of Systematic Reviews (2).
- Edwards SP, et al. (2007). Cleft lip and palate. In DM Laskin, AO Abubaker, eds., Oral and Maxillofacial Surgery, pp. 135–151. Chicago: Quintessence Publishing.
- Hoffman WY (2012). Cleft lip and palate. In AK Lalwani, ed., Current Diagnosis and Treatment in Otolaryngology—Head and Neck Surgery, 3rd ed., pp. 345–361. New York: McGraw-Hill.
- Klein U (2014). Oral medicine and dentistry. In WW Hay Jr et al., eds., Current Diagnosis and Treatment: Pediatrics, 21st ed., pp. 490–501. New York: McGraw-Hill.
- Mossey PA, et al. (2009). Cleft lip and palate. Lancet, 374(9703): 1773–1785.
- Porter RS, et al., eds. (2011). Congenital craniofacial and musculoskeletal abnormalities. In Merck Manual of Diagnosis and Therapy, 19th ed., pp. 2969–2975. Whitehouse Station, NJ: Merck Sharp and Dohme Corp.
- Rowe LD (2009). Congenital disorders of the oral cavity and lip section of Congenital anomalies of the head and neck. In JB Snow Jr, PA Wackym, eds., Ballenger’s Otorhinolaryngology Head and Neck Surgery, 17th ed., pp. 835–838. Hamilton, ON: BC Decker.
- Shi M, et al. (2007). Orofacial cleft risk is increased with maternal smoking and specific detoxification-gene variants. American Journal of Human Genetics, 80(1): 76–90.
Current as of: December 12, 2018
Author: Healthwise Staff
Medical Review:John Pope, MD, MPH – Pediatrics & Kathleen Romito, MD – Family Medicine & Adam D. Schaffner, MD, FACS – Plastic Surgery, Otolaryngology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.