Congenital Hydrocephalus
Topic Overview
What is congenital hydrocephalus?
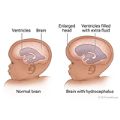
Congenital hydrocephalus is a buildup of excess cerebrospinal fluid (CSF) in the brain at birth. The extra fluid can increase pressure in the baby’s brain, causing brain damage and mental and physical problems. This condition is rare.
Finding the condition early and treating it quickly can help limit any long-term problems. But long-term effects mostly depend on what caused the fluid buildup, how bad it gets, and how the baby responds to treatment.
When hydrocephalus doesn’t occur until later in life, it is called acquired hydrocephalus. This topic focuses on hydrocephalus that is present at birth (congenital).
What causes congenital hydrocephalus?
This condition is caused by an imbalance between how much fluid the brain makes and how well the body is able to process it.
Normally, fluid flows through and out of chambers of the brain called ventricles, and then around the brain and spinal cord. The fluid is then absorbed by the thin tissue around the brain and spinal cord. But with hydrocephalus, the fluid can’t move where it needs to or is not absorbed as it should be. And in rare cases the brain makes too much fluid.
Congenital hydrocephalus may happen because of:
- Bleeding in the fetus before birth.
- Certain infections in the mother, such as toxoplasmosis or syphilis.
- Other birth defects, like spina bifida.
- A genetic defect.
What are the symptoms?
The clearest symptom of hydrocephalus is a head that is larger than normal. You and your doctor may notice it when the baby is born or within the first several months of life. It’s normal for a baby’s head to grow a lot during the first year. But with congenital hydrocephalus, the head may grow faster than the normal rate for a baby’s height and weight.
The condition may cause the soft spot (fontanelle) on your baby’s head to feel firm or bulge out. Also, the areas between the skull bones (sutures) may be larger than normal.
If pressure builds in the brain, your baby may:
- Be irritable.
- Sleep too much.
- Vomit.
- Eat very little.
How is congenital hydrocephalus diagnosed?
A fetal ultrasound can sometimes show the problem before birth. But most cases are found during a physical exam soon after birth. Your doctor may suspect that your baby has congenital hydrocephalus if your baby’s head is larger than normal.
Your baby may need imaging tests, such as a CT scan, an MRI, or an ultrasound, that can give a picture of the brain with more detail. Genetic tests may be done in some cases.
How is it treated?
Early treatment—before age 4 months—is important to help limit or prevent brain damage. Treatment focuses on reducing the amount of fluid in the brain to relieve pressure.
In most cases, the doctor places a flexible tube, called a shunt, in the brain to drain the fluid. The shunt carries fluid to another part of the body (usually the belly or the heart), which then absorbs the fluid. The shunt may stay in the brain for life, though it may have to be fixed or replaced later if it becomes blocked or infected.
A surgery called endoscopic third ventriculostomy (ETV) may be used instead of a shunt in some cases. In ETV, a small hole is made in the deep part of the brain so that the fluid in the brain can flow freely.
Sometimes emergency treatment is needed to reduce the fluid. This may include medicines, a lumbar puncture (sometimes called a spinal tap), or a procedure to drain fluid from the brain until a shunt can be put in.
If your child has any developmental problems or delays caused by damage to the brain, your doctor can help you find the care you need. Treatment will focus on the specific problems your child has. For example, speech therapy can help with speech delays. Physical therapy can help with motor skill problems.
What kind of ongoing care will your child need?
No matter what kind of treatment your child has had, you and your child’s doctors will need to watch your child closely to make sure that the fluid in the brain continues to drain properly. Pressure can build up in the brain again. Shunts can become blocked or infected. These problems need to be treated right away to prevent permanent damage.
Symptoms such as irritability, poor appetite, sleeping too much, and vomiting often may be signs that fluid has built up again in your child’s brain. After early childhood, there may be other symptoms to watch for, such as headaches, vision problems, confusion, slurred speech, or problems walking. Shunt infections may also cause a fever and redness along the shunt tract or valve.
As your child grows, you’ll need to watch for problems with brain development. These could include things like delayed learning, problems with motor skills, and speech problems. Talk to your doctor about any new problems or changes you notice.
It can be hard to wait and see if symptoms will return. And if your child has special needs, it can be a challenge to take care of him or her. Try to take good care of yourself. And ask your doctor about support groups and organizations that can help.
References
Other Works Consulted
- Feldstein NA, Anderson R (2006). Diagnosis and management of hydrocephalus. In FD Burg et al., eds., Current Pediatric Therapy, 18th ed., pp. 374–377. Philadelphia: Saunders Elsevier.
- Kinsman SL, Johnston MV (2011). Congenital anomalies of the central nervous system. In RM Kliegman et al., eds., Nelson Textbook of Pediatrics, 19th ed., pp. 1998–2013. Philadelphia: Saunders.
- Prockop LD (2010). Hydrocephalus. In LP Rowland, TA Pedley, eds., Merritt’s Neurology, 12th ed., chap. 53, pp. 349–355. Philadelphia: Lippincott Williams and Wilkins.
- Ropper AH, et al. (2014). Disturbances of cerebrospinal fluid and its circulation, including hydrocephalus, pseudotumor cerebri, and low-pressure syndromes. In Adams and Victor’s Principles of Neurology, 10th ed., pp. 617–638. New York: McGraw-Hill Education.
- Seiff ME (2003). Hydrocephalus section of Developmental, neurocutaneous, and genetic metabolic disorders. In RW Evans, ed., Saunders Manual of Neurologic Practice, pp. 889–895. Phildelphia: Saunders.
- Ulrich NJ (2011). Hydrocephalus and pseudotumor cerebri. In CD Rudolph et al., eds., Rudolph’s Pediatrics, 22nd ed., pp. 2174–2178. New York: McGraw-Hill.
Current as of: December 12, 2018
Author: Healthwise Staff
Medical Review:John Pope, MD, MPH – Pediatrics & E. Gregory Thompson, MD – Internal Medicine & Kathleen Romito, MD – Family Medicine & Christian G. Zimmerman, MD, FACS, MBA – Neurological Surgery
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.