Food Allergies
Topic Overview
Is this topic for you?
This topic has general information about food allergies. If you would like more specific information about peanut allergy, see the topic Peanut Allergy.
What is a food allergy?
When you have a food allergy, your body thinks certain foods are trying to harm you. Your body fights back by setting off an allergic reaction. In most cases, the symptoms are mild—a rash or an upset stomach. A mild reaction is no fun, but it isn’t dangerous. A serious reaction can be deadly. But quick treatment can stop a dangerous reaction.
Allergies tend to run in families. You are more likely to have a food allergy if other people in your family have allergies like hay fever, asthma, or eczema (atopic dermatitis).
Food allergies are more common in children than in adults. Children sometimes outgrow their food allergies, especially allergies to milk, eggs, or soy. But if you develop a food allergy as an adult, you will most likely have it for life.
Food allergy versus food intolerance
Food intolerances are much more common than food allergies. True food allergies are a reaction to food or food additives by your body’s immune system.
Many people think they have a food allergy, but in fact they have a food intolerance. Food intolerance is much more common. It can cause some of the same symptoms as a mild food allergy, like an upset stomach. But a food intolerance does not cause an allergic reaction. A food intolerance can make you feel bad, but it is not dangerous. A serious food allergy can be dangerous.
What are the symptoms?
Food allergies can cause many different symptoms. They can range from mild to serious. If you eat a food you are allergic to:
- Your mouth may tingle, and your lips may swell as you start to eat the food.
- You may have a stuffy nose, wheeze, or be short of breath when the allergens reach your mouth and lungs.
- You may have cramps, an upset stomach, or diarrhea as the food is digested.
- You may feel dizzy or lightheaded if your blood pressure drops as the allergens circulate through your bloodstream.
- You may have itchy skin with red, raised bumps called hives as the allergens reach your skin.
Kids usually have the same symptoms as adults. But sometimes a small child just cries a lot, vomits, has diarrhea, or does not grow as expected. If your child has these symptoms, see your doctor.
Some people have symptoms after eating even a tiny bit of a problem food. As a rule, the sooner the reaction begins, the worse it will be.
The most severe reaction is called anaphylaxis (say “ANN-uh-fuh-LAK-suss”). It affects your whole body. Anaphylaxis can start within a few minutes to a few hours after you eat the food. And the symptoms can go away and come back hours later. If you have anaphylaxis:
- Your throat and tongue may swell quickly.
- You may suddenly start wheezing or have trouble breathing.
- You may feel sick to your stomach or vomit.
- You may feel faint or pass out.
Anaphylaxis can be deadly. If you have (or see someone having) any of these symptoms, call 911 right away.
What foods most often cause a food allergy?
A few foods cause most allergies. The protein in a food that causes an allergy is called a food allergen.
- Milk, eggs, peanuts, tree nuts, fish, shellfish, wheat, and soy cause most problems in children.
- Milk, peanuts, tree nuts, fish, and shellfish cause most problems in adults.
If you are allergic to one food, you may also be allergic to other foods like it. So if you are allergic to shrimp, you may also be allergic to lobster or crab.
How is a food allergy diagnosed?
Your doctor will ask questions about your medical history and any family food allergies. And he or she will do a physical exam. Your doctor will also ask what symptoms you have. He or she may want you to write down everything you eat and any reactions you have. Your doctor will consider other possibilities that could be confused with food allergies, such as a food intolerance.
Because food allergies can be confused with other problems, it is important for your doctor to do a test to confirm that you have a food allergy. Your doctor may first start out with either skin testing or a blood test to determine what you are allergic to. But an oral food challenge is the best way to diagnose a food allergy. In an oral food challenge, you will eat a variety of foods that may or may not cause an allergic reaction. Your doctor watches to see if and when a reaction occurs.
A skin prick test can help to find out which foods will cause a reaction. The doctor will put a little bit of liquid on your skin and then prick your skin. The liquid has some of the possible food allergen in it. If your skin swells up like a mosquito bite, your doctor knows that you are allergic to that food. Your doctor may also do blood tests to look for the chemicals in your blood that cause an allergic reaction.
How is it treated?
The best treatment is to never eat the foods you are allergic to. Learn to read food labels and spot other names for problem foods. For example, milk may be listed as “caseinate,” wheat as “gluten,” and peanuts as “hydrolyzed vegetable protein.” When you eat out or at other people’s houses, ask about the foods you are served.
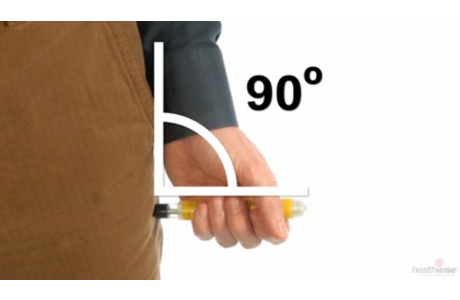
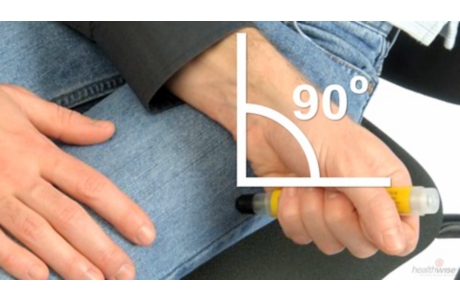
If you have a history of severe food allergies, your doctor will prescribe epinephrine (say “eh-puh-NEH-fren”). An epinephrine shot can slow down or stop an allergic reaction. Your doctor can teach you how to give yourself the shot if you need it.
You can have symptoms again even after you give yourself a shot. So go to the emergency room every time you have a severe reaction. You will need to be watched for several hours after the reaction.
If you have had a serious reaction in the past, your chance of having another one is high. Be prepared.
- Keep epinephrine with you at all times.
- Wear a medical alert bracelet to let others know about your food allergy.
- Check the expiration date on the epinephrine. Replace it as needed.
If your child has a food allergy, what else should you think about?
Talk to your child’s teachers and caregivers. They should know how to keep problem foods away from your child. Teach them what to do if your child eats one of these foods by mistake.
If your child has ever had a severe reaction, keep epinephrine nearby at all times. Some kids carry it in a fanny pack. Have your child wear a medical alert bracelet. Teach all caregivers to act quickly. They should:
- Know the signs of a severe reaction.
- Know how to give an epinephrine shot.
- Call 911 right away.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Cause
Food allergies occur when the body’s immune system overreacts to substances in food you have eaten, triggering an allergic reaction. Food allergies are more common in young children than in adults.
- Milk, eggs, peanuts, tree nuts, fish, shellfish, wheat, and soy cause most problems in children. Some babies are so sensitive to these foods that if the offending food is eaten by the mother, drinking her breast milk can cause a reaction. Most children outgrow allergies to eggs, milk, wheat, and soy.
- Peanuts, tree nuts, fish, and shellfish cause most of the allergic reactions in teens and adults. Adults typically remain allergic to the food for life.
Food allergies are most common in people who are atopic, meaning they have an inherited tendency to have allergic conditions. These people are more likely to have asthma, various allergies, and a skin condition called atopic dermatitis. Asthma can make the reaction to a food more severe.
If you are highly sensitive to a certain food, you may have an allergic reaction simply by being near where the food was prepared or served.
Celiac disease is an abnormal immune system reaction to gluten, a protein found in grains like wheat and rye. It damages the small intestine so that it can’t do a good job of absorbing nutrients from your food. For more information, see the topic Celiac Disease.
Cross-reactivity
Many people, but not all people, are allergic to foods that are similar or somehow related. This is called cross-reactivity. For example, if you are allergic to shrimp, you may also be allergic to other shellfish, like crab or lobster. If you are allergic to peanuts, you may be allergic to other members of the legume family, such as peas and beans. You don’t need to stop eating a cross-reactive food if you show no signs of an allergic reaction to it.
Oral allergy syndrome is a type of cross-reactivity. With this syndrome, people who have pollen allergies (such as a grass allergy) may develop itching, redness, and swelling of the lips and mouth when they eat fruits or vegetables that contain a protein that reacts with the pollen. These symptoms usually resolve quickly and do not involve other parts of the body.
Oral allergy syndrome usually involves a reaction to fresh fruits and raw vegetables:
- If you are allergic to ragweed, your mouth may itch when you eat melons, especially cantaloupe.
- If you are allergic to birch pollen, you may react to apple peels.
A growing number of people, especially health care workers, are discovering that they have an allergy to latex. Latex is the natural sap of the rubber tree. It is used in making surgical gloves, condoms, balloons, and other products. If you have a latex allergy, you may also have allergies to bananas, avocados, kiwi, and chestnuts.
Other concerns
Some people have allergic reactions to food after they exercise. This is called exercise-induced food allergy. As a person’s body temperature rises with exercise, symptoms such as itching and lightheadedness start, sometimes leading to hives and even anaphylaxis, which can be deadly. To avoid exercise-induced food allergy, do not eat for a few hours before you exercise or right after exercising.
Symptoms
Symptoms of food allergy can affect many parts of your body, including your:
- Digestive system. Symptoms include stomach cramps, nausea, vomiting, diarrhea, itching in the mouth and throat, and rectal bleeding (rare in adults). These symptoms occur more often in children than in adults.
- Skin. Symptoms include hives or welts, swelling, itching, redness, and atopic dermatitis. Skin reactions are common in children. If your baby has atopic dermatitis, you may help prevent peanut allergies by introducing peanut products early.
- Respiratory system. Symptoms include coughing; wheezing; an itchy, stuffy, runny nose; sneezing; and trouble breathing.
Children usually have the same symptoms as adults. Symptoms of milk or soy allergies in children may include eczema. Sometimes the only symptoms are extreme crying, vomiting, blood in the stool, diarrhea, constipation, or poor growth.
Symptoms vary from mild to life-threatening and can appear from within minutes to days of eating a food. The most severe reaction is anaphylaxis, which affects many body systems and can be deadly.
Anaphylaxis can start within a few minutes to a few hours after you eat the food. And the symptoms can go away and come back hours later. Common triggers for anaphylaxis are peanuts, nuts, and seafood. In children, peanuts cause anaphylaxis more often than other foods. Aspirin, exercise, or alcohol can increase the risk for anaphylaxis.
There are many other conditions with similar symptoms, such as food poisoning and inflammatory bowel disease.
What Happens
The first time you eat a food that triggers an allergic reaction, your body’s immune system recognizes the food as a foreign substance (allergen). Your body reacts by developing antibodies against the food. When you eat the offending food again, the antibodies attack the allergen, releasing histamine and other chemicals that cause the symptoms of an allergic reaction.
To learn more, see the Symptoms and Treatment Overview sections of this topic.
What Increases Your Risk
You have a greater chance of developing food allergies if you:
- Have a family history of allergy. If both of your parents have allergies, you are more likely to have allergies.
- Have another allergic condition such as atopic dermatitis or asthma.
- Are young. Infants and children have more food allergies than adults.
- Have a medical condition that makes it easier for allergens to pass through the walls of the stomach and intestines and enter the bloodstream. These conditions include gastrointestinal disease, malnutrition, prematurity, and diseases that impair the immune system, such as eosinophilic esophagitis (EoE).
You have a greater risk for a life-threatening allergic reaction (anaphylaxis) from food allergy if you:
- Have asthma.
- Develop allergy symptoms within minutes of eating the food.
If you or your child has a severe food allergy, always carry epinephrine and know how to use it. You should also wear a medical alert bracelet at all times. Being prepared to immediately deal with a severe allergic reaction reduces the risk of death.
When should you call your doctor?
Give an epinephrine shot if:
- You think you are having a severe allergic reaction.
- You have symptoms in more than one body area, such as mild nausea and an itchy mouth.
After giving an epinephrine shot call 911, even if you feel better.
Call 911 if you have:
- Rapid swelling of the throat or tongue
- Trouble breathing, wheezing, or deep cough; a pale face or blue lips or earlobes
- Feeling faint
- Signs of shock, including:
- Lightheadedness or a feeling that you are about to pass out
- Restlessness, confusion, or a sense of impending doom
- Moist, cool skin, or possibly profuse sweating
- Weakness, thirst, nausea, or vomiting
- Been given an epinephrine shot, even if you feel better.
If you witness a severe allergic reaction and the person becomes unconscious, call 911 or other emergency services immediately.
If your food allergy symptoms are getting worse, call your doctor. It is important to know which foods are to blame so that you can avoid them.
Watchful waiting
If your food allergy symptoms do not get worse or are not too severe or bothersome, you can try eliminating suspect foods from your diet to see whether symptoms disappear.
Who to see
The following health professionals may evaluate and treat mild food allergies:
An allergy specialist may be needed when:
- You need to identify the foods that trigger allergic reactions.
- Your work or school performance or quality of life is affected because of allergy symptoms or medicine side effects.
- You have other medical conditions, such as recurrent asthma.
You may also be referred to other specialists, such as a:
- Dermatologist, to treat allergic skin problems.
- Pulmonary specialist, when moderate or severe asthma is also present.
A registered dietitian can help you keep a balanced diet even when you can’t eat some foods. A dietitian can also help you learn how to avoid hidden allergens in foods and give you ideas about how to make substitutions in recipes.
Exams and Tests
To diagnose a food allergy, your doctor will start with a medical history and a physical exam. Your doctor may ask:
- What symptoms you have.
- If your family has any food allergies.
- How soon the symptoms began after eating food.
- If over-the-counter medicines helped.
- If other people also got sick.
- How the food was prepared.
- If you ate any other foods.
It’s important to find out whether you have a food allergy or food intolerance. Your doctor may ask you to keep a record of all the foods you eat and any reactions you have to them. Your doctor will also consider if your reaction could have been caused by things like allergies to medicines or insect stings, food poisoning, irritants in foods, or exposure to skin irritants.
Your doctor may ask you to try an elimination diet, an oral food allergy challenge, or both.
- In an elimination diet, you avoid eating foods that may be causing an allergic reaction and see if your symptoms go away. If symptoms come back when you eat the food again, your doctor can confirm your food allergy. The elimination diet can last from 2 to 8 weeks.
- In an oral food allergy challenge, you eat a variety of foods that may or may not cause an allergic reaction. Your doctor watches to see if and when a reaction occurs. This test is considered the best way to diagnose a food allergy.
After you have been diagnosed with a food allergy, you may also have allergy tests, such as skin tests or blood tests, to find out which foods you are allergic to.
Treatment Overview
The best treatment for food allergies is to avoid the food that causes the allergy. When that isn’t possible, you can use medicines such as antihistamines for mild reactions and epinephrine for serious reactions. Talk to your doctor about an Anaphylaxis Action Plan.
Start by telling your family, friends, and coworkers that you have a food allergy, and ask them to help you avoid the food. Read all food labels, and learn the other names that may be used for food allergens.
If your baby has a milk or soy allergy, your doctor may suggest either that you change the formula or that you feed your baby only breast milk. Specially prepared formulas are available for infants who have soy and milk allergies.
If you have a severe allergic reaction, your first treatment may be done in an emergency room or by emergency personnel. You will be given a shot of epinephrine to stop the further release of histamine and to relax the muscles that help you breathe.
How to treat a reaction
If your doctor has prescribed epinephrine, always keep it with you. It’s important to give the epinephrine shot right away. Your doctor or pharmacist will teach you how to give yourself a shot if you need it. Be sure to check the expiration dates on the medicines, and replace the medicines as needed.
For step-by-step instructions on how to give the shot, see:
You should also wear a medical alert bracelet or other jewelry that lists your food allergies. You can order medical alert jewelry through most drugstores or on the Internet.
Research for new treatments
Food oral immunotherapy (OIT) is being studied as a way to help treat food allergies. Under close supervision, a person takes in small daily doses of a food allergen by mouth or under the tongue. The goal is to try to make the immune system tolerate the allergen so that the body won’t react as badly to it. This is called desensitization. Talk to your doctor if you want to know more about clinical trials for this and other new treatments being studied.
Children and food allergies
It’s important to take special care with children who have food allergies. A child with severe food allergies may have a life-threatening anaphylactic reaction to even a tiny amount of a food allergen. Your child should always wear a medical alert bracelet. Talk to your doctor about an Anaphylaxis Action Plan.
Make sure that all caregivers (school administrators, teachers, friends, coaches, and babysitters):
- Know about your child’s food allergy.
- Can recognize the symptoms of a food allergy.
- Know where the epinephrine shot is kept and how to use it.
- Know to call 911 immediately.
Children may have only mild symptoms in the first few minutes after they eat the food allergen, but they may have severe symptoms in 10 to 60 minutes. Children always should be observed in a hospital for several hours after a reaction.
Make sure that your child:
- Always wears a medical alert bracelet.
- Always carries epinephrine. Children at risk of severe allergic reactions should keep their epinephrine at school or day care and at home. Older, mature children should be taught to give themselves the shot.
Although your child needs to avoid certain foods, he or she still needs to eat healthy foods. A dietitian can tell you which foods are important for your child’s health.
Prevention
Food allergies often occur in people who have a family history of asthma, atopic dermatitis, or allergies to pollen, mold, or other substances. In most cases, allergies cannot be prevented in people who have a family history of allergic conditions.
There isn’t enough proof to recommend that people who are at risk for allergies should avoid common foods that cause allergies like milk, eggs, peanuts, tree nuts, soy, wheat, fish, shellfish, and sulphites. Avoiding these foods doesn’t seem to prevent allergies.
If your doctor thinks your baby might be at risk for a peanut allergy, ask him or her about introducing peanut products. There may be a way to prevent peanut allergies.footnote 1
If you are a woman with a food allergy who is planning on a pregnancy and breastfeeding, talk to your doctor about what foods to avoid while pregnant or nursing. But if you don’t have food allergies, avoiding certain foods during your pregnancy isn’t recommended as a way to prevent the baby from having food allergies.
The American Academy of Pediatrics recommends that all babies be breastfed for the first year of life or longer.footnote 1 For babies with family members who have food allergies, ask whether and how to start foods that might cause allergies. Most allergic reactions in children are caused by eggs, milk, wheat, soy, and peanuts. Breastfeeding only for at least 4 months may help prevent allergies to milk.footnote 2 If your baby is at high risk for allergies and you can’t breastfeed, try a hydrolyzed milk formula. The milk protein in hydrolyzed formulas is changed to try to prevent allergies. There is no proof that giving your baby soy formula instead of cow’s milk formula will prevent a food allergy in children at risk for food allergies.footnote 2
Tobacco smoke can make allergies worse, so it is important to have a smoke-free environment.
Home Treatment
Knowing which foods trigger food allergies and avoiding those foods is the best way to prevent allergic reactions. Unfortunately, food allergens are often hidden in sauces, ice creams, baked goods, and other items.
If you have food allergies, read food labels carefully.
Sometimes products are recalled when food ingredients are missing from food labels. For a list of recalled products, see the U.S. Food and Drug Administration’s Recalls, Market Withdrawals, and Safety Alerts page at www.fda.gov/opacom/7alerts.html.
Tips for eating out
Eating out can be dangerous for people with severe food allergies.
- Bring safe substitutes from home. For example, bring soy milk to have with cereal.
- Be aware of possible cross-contamination. For example, an ice cream scoop may have been used for Rocky Road ice cream, which contains peanuts, and then used for your vanilla ice cream.
- Alert the wait staff to the possibility of a severe food reaction. Carefully question them about ingredients. If they are not sure, ask to speak to kitchen staff.
- Always wear medical alert jewelry that lists your food allergies. Medical alert jewelry can be ordered through most drugstores or on the Internet.
If you or your child has ever had a severe allergic reaction, always carry an epinephrine shot.
If you are traveling to another country, learn the words for the foods that trigger your allergy so that you can ask in restaurants and read food labels. Call airlines, tour operators, and restaurants ahead of time to explain your food allergy and request safe meals. Prepare your own food when possible. Discuss your travel plans with your doctor.
Medications
Medicine is used to treat some food allergies.
For mild allergic reactions, people often try nonprescription medicines first. You can try prescription medicines if over-the-counter medicines fail to control allergy symptoms or if they cause drowsiness or other bothersome side effects.
Medicine choices
Medicines used to treat a severe allergic reaction include:
- Epinephrine. Epinephrine is given as a shot. It acts quickly to relax the muscles that help you breathe. Sometimes more than one shot is needed if symptoms do not go away. Epinephrine is the medicine used to treat anaphylaxis.
- Antihistamines. Antihistamines block the action of histamine during an allergic reaction and help improve symptoms such as itching and sneezing.
- Corticosteroids. These medicines help reduce inflammation.
Medicines used to relieve mild food allergy symptoms include:
- Antihistamines and corticosteroids for hives, gastrointestinal symptoms, or sneezing and a runny nose.
- Bronchodilators for asthma symptoms. Bronchodilators relax the airways of the lungs, making it easier to breathe.
References
Citations
- American Academy of Pediatrics (2012). Policy statement: Breastfeeding and the use of human milk. Pediatrics, 129(3): e827–e841. Also available online: http://pediatrics.aappublications.org/content/129/3/e827.full.
- Greer FR, et al. (2008). Effects of early nutritional interventions on the development of atopic disease in infants and children: The role of maternal dietary restriction, breastfeeding, timing of introduction of complementary foods, and hydrolyzed formulas. Pediatrics, 121(1): 183–191. Also available online: http://pediatrics.aappublications.org/content/121/1/183.full.
Other Works Consulted
- American Academy of Allergy, Asthma, and Immunology (2010). Guidelines for the diagnosis and management of food allergy in the United States: Report of the NIAID-sponsored expert panel. Journal of Allergy and Clinical Immunology, 126(6): S1–S58. Available online: http://www.niaid.nih.gov/topics/foodallergy/clinical/Pages/default.aspx.
- Branum AM, Lukacs SL (2008). Food allergy among U.S. children: Trends in prevalence and hospitalizations. National Center for Health Statistics Data Brief, No. 10. Hyattsville, MD: National Center for Health Statistics. Available online: http://www.cdc.gov/nchs/data/databriefs/db10.pdf.
- Drugs for allergic disorders (2010). Treatment Guidelines From The Medical Letter, 8(90): 9–18.
- Greenhawt M (2013). Food allergies. In EG Nabel, ed., ACP Medicine, section 3, chap. 8. Hamilton, ON: BC Decker.
- Katz DL, Friedman RSC (2008). Food allergy and intolerance. In Nutrition in Clinical Practice, pp. 275–280. Philadelphia: Lippincott Williams and Wilkins.
- Longo G, et al (2013). IgE-mediated food allergy in children. Lancet, 382(9905): 1656–1664. DOI: 10.1016/S0140-6736(13)60309-8. Accessed November 26, 2013.
- Sampson H, et al. (2014). Food allergy: A practice parameter update—2014. Journal of Allergy Clinical Immunology, 134(5): 1016. http://www.aaaai.org/Aaaai/media/MediaLibrary/PDF%20Documents/Practice%20and%20Parameters/Food-Allergy-A-Practice-Parameter-Update-2014.pdf. Accessed February 19, 2015.
- Sampson HA (2003). Adverse reactions to foods. In NF Adkinson et al., eds., Middleton’s Allergy Principles and Practice, 6th ed., vol. 2, pp. 1619–1643. Philadelphia: Mosby.
- Skripak JM, Sampson HA (2008). Towards a cure for food allergy. Current Opinion in Immunology, 20: 690–696.
Current as of: April 7, 2019
Author: Healthwise Staff
Medical Review:E. Gregory Thompson MD – Internal Medicine & Adam Husney MD – Family Medicine & Martin J. Gabica MD – Family Medicine & Kathleen Romito MD – Family Medicine & Rohit K Katial MD – Allergy and Immunology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.