Top of the pageCheck Your Symptoms
Puncture Wounds
Topic Overview
Causes of puncture wounds
A puncture wound is a forceful injury caused by a sharp, pointed object that penetrates the skin. A puncture wound is usually narrower and deeper than a cut or scrape. Many people accidentally get puncture wounds with household or work items, yard tools, or when operating machinery. Most puncture wounds are minor, and home treatment is usually all that is needed.
Sharp objects, such as nails, tacks, ice picks, knives, teeth, and needles, can all cause puncture wounds. Puncture wounds increase your risk of infection because they are hard to clean and provide a warm, moist place for bacteria to grow. The bacteria Pseudomonas are a common cause of infections when a puncture wound occurs through the sole of an athletic shoe.
Some punctures are done for health reasons. For example, a puncture may be used by a doctor to draw blood or to give fluid or medicines directly into a vein (intravenous, or IV).
Health professionals have an increased risk of needle-stick injuries. A puncture from a used needle increases the risk of infection or for transmitting a blood-borne disease, such as hepatitis or human immunodeficiency virus (HIV). Home treatment may be all that is needed for puncture wounds from clean needles.
What to do if you get a puncture wound?
When you have a puncture wound:
- Determine if any part of the object that caused the wound is still in the wound, such as a splinter or lead (graphite) from a pencil. A pencil lead puncture wound is less worrisome, so it is not necessary to check blood levels for lead or worry about lead toxicity or poisoning.
- Determine if underlying tissues, such as blood vessels, nerves, tendons, ligaments, bones, joints, or internal organs, have been injured by the object.
- Clean the wound and remove any dirt or debris to prevent infections, both bacterial skin infections and tetanus (“lockjaw”).
- Determine whether you need a tetanus shot.
Check your symptoms to decide if and when you should see a doctor.
Check Your Symptoms
The medical assessment of symptoms is based on the body parts you have.
- If you are transgender or nonbinary, choose the sex that matches the body parts (such as ovaries, testes, prostate, breasts, penis, or vagina) you now have in the area where you are having symptoms.
- If your symptoms aren’t related to those organs, you can choose the gender you identify with.
- If you have some organs of both sexes, you may need to go through this triage tool twice (once as “male” and once as “female”). This will make sure that the tool asks the right questions for you.
Many things can affect how your body responds to a symptom and what kind of care you may need. These include:
- Your age. Babies and older adults tend to get sicker quicker.
- Your overall health. If you have a condition such as diabetes, HIV, cancer, or heart disease, you may need to pay closer attention to certain symptoms and seek care sooner.
- Medicines you take. Certain medicines, herbal remedies, and supplements can cause symptoms or make them worse.
- Recent health events, such as surgery or injury. These kinds of events can cause symptoms afterwards or make them more serious.
- Your health habits and lifestyle, such as eating and exercise habits, smoking, alcohol or drug use, sexual history, and travel.
Try Home Treatment
You have answered all the questions. Based on your answers, you may be able to take care of this problem at home.
- Try home treatment to relieve the symptoms.
- Call your doctor if symptoms get worse or you have any concerns (for example, if symptoms are not getting better as you would expect). You may need care sooner.
Symptoms of infection may include:
- Increased pain, swelling, warmth, or redness in or around the area.
- Red streaks leading from the area.
- Pus draining from the area.
- A fever.
Pain in adults and older children
- Severe pain (8 to 10): The pain is so bad that you can’t stand it for more than a few hours, can’t sleep, and can’t do anything else except focus on the pain.
- Moderate pain (5 to 7): The pain is bad enough to disrupt your normal activities and your sleep, but you can tolerate it for hours or days. Moderate can also mean pain that comes and goes even if it’s severe when it’s there.
- Mild pain (1 to 4): You notice the pain, but it is not bad enough to disrupt your sleep or activities.
Pain in children under 3 years
It can be hard to tell how much pain a baby or toddler is in.
- Severe pain (8 to 10): The pain is so bad that the baby cannot sleep, cannot get comfortable, and cries constantly no matter what you do. The baby may kick, make fists, or grimace.
- Moderate pain (5 to 7): The baby is very fussy, clings to you a lot, and may have trouble sleeping but responds when you try to comfort him or her.
- Mild pain (1 to 4): The baby is a little fussy and clings to you a little but responds when you try to comfort him or her.
Certain health conditions and medicines weaken the immune system’s ability to fight off infection and illness. Some examples in adults are:
- Diseases such as diabetes, cancer, heart disease, and HIV/AIDS.
- Long-term alcohol and drug problems.
- Steroid medicines, which may be used to treat a variety of conditions.
- Chemotherapy and radiation therapy for cancer.
- Other medicines used to treat autoimmune disease.
- Medicines taken after organ transplant.
- Not having a spleen.
With severe bleeding, any of these may be true:
- Blood is pumping from the wound.
- The bleeding does not stop or slow down with pressure.
- Blood is quickly soaking through bandage after bandage.
With moderate bleeding, any of these may be true:
- The bleeding slows or stops with pressure but starts again if you remove the pressure.
- The blood may soak through a few bandages, but it is not fast or out of control.
With mild bleeding, any of these may be true:
- The bleeding stops on its own or with pressure.
- The bleeding stops or slows to an ooze or trickle after 15 minutes of pressure. It may ooze or trickle for up to 45 minutes.
You may need a tetanus shot depending on how dirty the wound is and how long it has been since your last shot.
- For a dirty wound that has things like dirt, saliva, or feces in it, you may need a shot if:
- You haven’t had a tetanus shot in the past 5 years.
- You don’t know when your last shot was.
- For a clean wound, you may need a shot if:
- You have not had a tetanus shot in the past 10 years.
- You don’t know when your last shot was.
Symptoms of difficulty breathing can range from mild to severe. For example:
- You may feel a little out of breath but still be able to talk (mild difficulty breathing), or you may be so out of breath that you cannot talk at all (severe difficulty breathing).
- It may be getting hard to breathe with activity (mild difficulty breathing), or you may have to work very hard to breathe even when you’re at rest (severe difficulty breathing).
Seek Care Today
Based on your answers, you may need care soon. The problem probably will not get better without medical care.
- Call your doctor today to discuss the symptoms and arrange for care.
- If you cannot reach your doctor or you don’t have one, seek care today.
- If it is evening, watch the symptoms and seek care in the morning.
- If the symptoms get worse, seek care sooner.
Seek Care Now
Based on your answers, you may need care right away. The problem is likely to get worse without medical care.
- Call your doctor now to discuss the symptoms and arrange for care.
- If you cannot reach your doctor or you don’t have one, seek care in the next hour.
- You do not need to call an ambulance unless:
- You cannot travel safely either by driving yourself or by having someone else drive you.
- You are in an area where heavy traffic or other problems may slow you down.
Call 911 Now
Based on your answers, you need emergency care.
Call911or other emergency services now.
Call 911 Now
Based on your answers, you need emergency care.
Call911or other emergency services now.
Put direct, steady pressure on the wound until help arrives. Keep the area raised if you can.
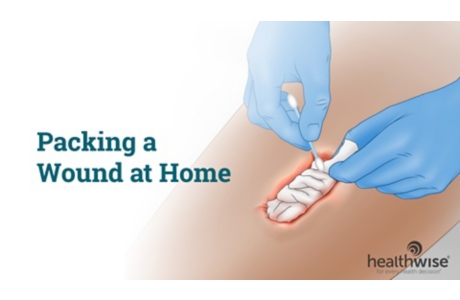
Home Treatment
Minor puncture wounds can be treated effectively at home. If you do not have an increased risk of infection, you do not have other injuries, and you do not need a tetanus shot or treatment by a doctor, you can treat a puncture wound at home. Home treatment can prevent infection and promote healing.
The American Red Cross recommends that everyone use blood and body fluid precautions with first aid treatment.
Remove object
- Make sure the object causing the wound is not still in the wound. Check to see if the object is intact and a piece has not broken off in the wound.
- Try to remove the object that caused the wound if it is small and you can see it. If you have a splinter, try using cellophane tape before using clean tweezers or a needle. Simply put the tape over the splinter, then pull the tape off. The splinter usually sticks to the tape and is removed painlessly and easily. Be careful, and do not push the object farther into the wound. Do not wet the splinter.
Stop the bleeding
- Allow the wound to bleed freely for up to 5 minutes to clean itself out, unless there has been a lot of blood loss or blood is squirting out of the wound.
- Stop the bleeding with direct pressure to the wound.
After you have stopped the bleeding, check your symptoms to determine if and when you need to see your doctor.
Clean the wound
Clean the wound as soon as possible to reduce the chance of infection, scarring, and tattooing of the skin from dirt left in the wound. (If dirt or other debris is not removed from a puncture wound, the new skin will heal over it. The dirt can then be seen through the skin and may look like a tattoo.)
- Wash the wound for 5 minutes with large amounts of cool water and soap (mild dishwashing soap, such as Ivory, works well). Some nonprescription products are available for wound cleaning that numb the area so cleaning doesn’t hurt as much. Be sure to read the product label for correct use.
- Do not use rubbing alcohol, hydrogen peroxide, iodine, or Mercurochrome, which can harm the tissue and slow healing.
Consider applying a bandage
Most puncture wounds heal well and don’t need a bandage. You may need to protect the puncture wound from dirt and irritation. Be sure to clean the wound thoroughly before bandaging it to reduce the risk of infection occurring under the bandage.
Puncture wounds are less likely than cuts to need stitches, staples or skin adhesives.
Tetanus
- Determine whether you need a tetanus shot.
- You may have a localized reaction to a tetanus shot. Symptoms include warmth, swelling, and redness at the injection site. A mild fever may occur. Home treatment can help reduce the discomfort.
Pain relief
Elevate the injured area on pillows anytime you are sitting or lying down. Try to keep the area at or above the level of your heart to reduce swelling.
|
Try a nonprescription medicine to help treat your fever or pain: |
|---|
Talk to your child’s doctor before switching back and forth between doses of acetaminophen and ibuprofen. When you switch between two medicines, there is a chance your child will get too much medicine. |
|
Be sure to follow these safety tips when you use a nonprescription medicine: |
|---|
|
Symptoms to watch for during home treatment
Call your doctor if any of the following occur during home treatment:
- Signs of infection
- Signs of loss of function
- Signs of decreased blood flow
- Pain gets worse.
- Symptoms become more severe or more frequent.
Prevention
To prevent puncture wounds, be sure to practice safety when using blunt or sharp objects.
- Pay close attention to what you are doing.
- If you become distracted, set the object aside until you can pay attention to what you are doing.
- Know how to use the object properly.
- Have good lighting so you can see what you are doing.
- Wear gloves whenever possible to protect your hands.
- Wear other safety gear, such as glasses or boots, as appropriate.
- Hold a sharp object away from your body while using it.
- Carry the object with the dangerous end away from you.
- Shut the power off and use safety locks on your power tools when you are not using them.
- Be very careful when using high-pressure equipment, such as staple guns or paint sprayers. Make sure your work area is clear of people and hazards that could interfere with the safe operation of the equipment.
- Store dangerous objects in secure places away from children.
- Teach children about safety, and be a good role model.
- Do not use alcohol or drugs when you are handling sharp objects.
Be sure to have a tetanus shot every 10 years.
Preparing For Your Appointment
To prepare for your appointment, see the topicMaking the Most of Your Appointment.
Questions to prepare for your appointment
You can help your doctor diagnose and treat your condition by being prepared to answer the following questions:
- What are your main symptoms? How long have you had your symptoms?
- How and when did the puncture wound occur? Have you had any injuries in the past to the same area? Do you have any continuing problems because of the previous injury?
- What object caused the puncture wound? Was there or is there an object in the puncture wound? Was the object removed in one piece? Did the injury occur under high pressure?
- What home treatment measures have you tried? Did they help?
- What nonprescription medicines have you tried? Did they help?
- What prescription and nonprescription medicine do you take?
- Were drugs or alcohol involved in your injury?
- When was your last tetanus shot?
- Do you have any health risks?
Current as of: June 26, 2019
Author: Healthwise Staff
Medical Review:William H. Blahd Jr. MD, FACEP – Emergency Medicine & Adam Husney MD – Family Medicine & Kathleen Romito MD – Family Medicine & H. Michael O’Connor MD – Emergency Medicine & Martin J. Gabica MD – Family Medicine
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.