Tonsillitis
Topic Overview

What is tonsillitis?
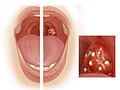
Tonsillitis is an infection or inflammation of the tonsils. The tonsils are balls of lymph tissue on both sides of the throat, above and behind the tongue. They are part of the immune system, which helps the body fight infection.
Tonsillitis often goes away on its own after 4 to 10 days.
What causes tonsillitis?
Most often, tonsillitis is caused by a virus. Less often, it is caused by the same bacteria that cause strep throat. In rare cases, a fungus or a parasite can cause it.
Tonsillitis is spread through the air in droplets when an infected person breathes, coughs, or sneezes. You may then become infected after breathing in these droplets or getting them on your skin or on objects that come in contact with your mouth, nose, or eyes.
What are the symptoms?
The main symptom of tonsillitis is a sore throat. The throat and tonsils usually look red and swollen. The tonsils may have spots on them or pus that covers them completely or in patches. Fever is also common.
If you feel like you have a cold, with symptoms such as runny and stuffy nose, sneezing, and coughing, a virus is most likely the cause.
If you have a sore throat plus a sudden and severe fever and swollen lymph nodes, but you do not have symptoms of a cold, the infection is more likely caused by bacteria. This means you need to see a doctor and probably need a strep test.
How is tonsillitis diagnosed?
Your doctor will look at your throat to see if you have red and swollen tonsils with spots or sores. These signs can mean you have tonsillitis.
Your doctor may do a rapid strep test along with a throat culture. These will show whether the tonsillitis is caused by streptococcus bacteria.
Your doctor may also ask about past throat infections. If you get tonsillitis often, it may affect the choice of treatment.
You may have a test for mononucleosis if your doctor thinks that you have mono.
How is it treated?
Tonsillitis caused by a virus will usually go away on its own. Treatment focuses on helping you feel better. You may be able to ease throat pain if you drink warm tea, take over-the-counter pain medicine, and use other home treatments. Do not give aspirin to anyone age 20 or younger. It is linked to a serious disease called Reye syndrome.
If your tonsillitis is caused by strep, you need treatment with antibiotics. Antibiotics can help prevent rare but serious problems caused by strep and can control the spread of infection.
As a rule, doctors only advise surgery to remove tonsils (tonsillectomy) when there are serious problems with the tonsils. These include infections that happen again and again or long-lasting infections that do not get better after treatment and get in the way of daily activities. You and your doctor can decide if surgery is the right choice after a careful review of your or your child’s overall health.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Cause
Tonsillitis is usually caused by a virus. Bacteria can also cause tonsillitis. The most common bacterial cause of tonsillitis is group A beta-hemolytic streptococcus (GABHS), which also causes strep throat.
Tonsillitis can also be caused by fungi or parasites. But these causes are rare in people who have healthy immune systems.
How tonsillitis is spread
Tonsillitis is spread by close contact with an infected person. Droplets of disease-causing agents (pathogens) pass through the air when an infected person breathes, coughs, or sneezes. You may then become infected after you breathe in these droplets. Infection can also occur if pathogens get on your skin or on objects that come in contact with your mouth, nose, eyes, or other mucous membranes. Symptoms usually appear about 2 to 5 days after exposure.
A person with tonsillitis caused by strep bacteria is contagious early on and, without treatment, can remain so for up to 2 weeks. Antibiotics shorten the contagious period, and an infected person is no longer contagious about 24 to 48 hours after beginning antibiotic therapy.
Symptoms
The main symptom of tonsillitis is a sore throat. More symptoms occur in most cases. Some or all of the following may be present:
- Fever
- Bad breath
- Nasal congestion and runny nose
- Swollen lymph nodes
- Red, swollen tonsils covered completely or in patches by pus
- Difficulty swallowing
- Headache
- Abdominal (belly) pain
- Raw, bleeding patches on the tonsils
When you have sore throat plus cold symptoms such as nasal congestion, runny nose, sneezing, and coughing, the cause is most likely a virus. Viral infection of the tonsils usually goes away without treatment within 2 weeks.
Sore throat with, swollen glands, a sudden fever above 101°F (38.3°C), and without symptoms of an upper respiratory tract infection may point to a bacterial infection like strep that needs to be treated with antibiotics.
What Happens
Tonsillitis, in most cases, lasts 4 to 10 days. A bacterial sore throat may last slightly longer but usually gets better with antibiotics.
In some cases, tonsillitis can become chronic. Surgical removal of the tonsils (tonsillectomy) may be recommended for you or your child based on past health and results of physical exams.
Complications of tonsillitis
Tonsillitis caused by strep bacteria that is not treated with antibiotics may result in complications, such as ear and sinus infections or pockets of infection outside the tonsils (peritonsillar abscess). More serious complications, such as rheumatic fever, are rare.
Recurrent and ongoing (chronic) tonsillitis may obstruct the upper airway and cause problems, such as snoring, nasal congestion, and mouth breathing. Sometimes chronic tonsillitis can lead to more severe conditions, including obstructive sleep apnea and heart and lung problems. But most children who have sleep apnea and enlarged tonsils do not have a history of tonsillitis.
What Increases Your Risk
Close contact with an infected person is the main risk factor for tonsillitis. Droplets of disease-causing agents (pathogens) pass through the air when an infected person breathes, coughs, or sneezes. You may then become infected after breathing in these droplets. Infection can also occur if pathogens get on your skin or on objects that come in contact with the mouth, nose, eyes, or other mucous membranes.
Nasal obstruction causes you to breathe through your mouth, which increases the risk of tonsillitis.
When should you call your doctor?
Call your doctor if any of the following occur.
- Sore throat, along with any two of these signs of bacterial infection:
- Fever of 101°F (38.3°C) or higher
- White or yellow coating on the tonsils
- Swollen, tender tonsils
- Swollen lymph nodes in the neck
- Rash
- Abdominal (belly) pain and headache
- Severe pain
- Severe difficulty swallowing
- Pain on only one side of the throat
- Tonsillitis or sore throat that starts after being exposed to someone who has strep throat.
- 7 episodes of tonsillitis in 1 year despite treatment.
- Persistent mouth-breathing, snoring, or a very nasal- or muffled-sounding voice.
- Signs of dehydration, such as a dry mouth and tongue and urinating less than normal.
Watchful waiting
Watchful waiting is a period of time during which you and your doctor observe your or your child’s symptoms or condition without using medical treatment. Watchful waiting is appropriate if tonsillitis occurs along with cold symptoms such as runny nose, nasal congestion, sneezing, and coughing. Tonsillitis with these symptoms is most often caused by a virus. Viral infection of the tonsils can be treated at home and in most cases goes away without treatment within 2 weeks. In general, the more like a cold the condition is, the less likely it is that the condition is caused by strep bacteria.
Watchful waiting is not appropriate if tonsillitis occurs with a fever of 101°F (38.3°C) or higher or with swollen lymph nodes in the neck, and without symptoms of an upper respiratory tract infection. If these symptoms occur together, see a doctor. You may have strep throat, which should be treated promptly.
Who to see
Health professionals who can evaluate tonsillitis, perform quick tests or throat cultures, and prescribe antibiotic treatment, if needed, include:
- Pediatrician
- Family medicine physician
- Otolaryngologist (ear, nose, and throat, or ENT, doctor)
- Nurse practitioner
- Physician assistant
- Internist
If surgery to remove the tonsils (tonsillectomy) is indicated, your doctor may refer you to an otolaryngologist (ear, nose, and throat, or ENT, doctor).
Exams and Tests
Diagnosis of tonsillitis is based on a medical history and a physical exam of the throat. An accurate medical history is needed to find out whether tonsillitis is recurrent, which may affect treatment choices.
If your symptoms suggest strep throat, your doctor may want to confirm this diagnosis by doing a throat culture. Strep throat is more likely if 3 or 4 of the following signs or symptoms are present:
- Fever
- White or yellow spots or coating on the throat and/or tonsils (tonsillar exudates)
- Swollen or tender lymph nodes on the neck
- Absence of coughing or sneezing
If a strep infection is suspected, your doctor may do a rapid strep test or a throat culture or both. Both of these tests can be done in a doctor’s office. You may want to discuss the advantages and disadvantages of each test to see which test is appropriate.
The results of these tests will determine whether antibiotic treatment is needed. These results combined with an accurate medical history will be considered in deciding whether surgery to remove the tonsils (tonsillectomy) is recommended.
If the Epstein-Barr virus, which can cause mononucleosis, is suspected as a cause for the tonsillitis, a test for mononucleosis may be done.
Treatment Overview
Tonsillitis is most often caused by a virus, which resolves on its own. But tonsillitis can be caused by strep bacteria, which requires treatment with antibiotics. Watch for signs of dehydration, such as a dry mouth and tongue. Also, watch for signs of complications, such as ear pain, from tonsillitis caused by strep bacteria.
Tonsillitis caused by a virus
Tonsillitis caused by a virus will usually go away on its own. Antibiotics are not effective treatment for viral tonsillitis.
The virus that causes mononucleosis (mono) can lead to tonsillitis that is as severe as tonsillitis caused by bacteria and can take several weeks or more before it goes away.
Home treatments such as drinking warm tea and taking over-the-counter pain medicine (such as acetaminophen or ibuprofen) may help relieve discomfort. Do not give aspirin to anyone younger than 20 because of its link to Reye syndrome, a serious but rare problem.
Many nonprescription remedies such as antiseptic mouthwashes, decongestants, and antihistamines contain extra ingredients that don’t relieve discomfort. These remedies are not recommended for children, because they have not been proved to have any benefits in the treatment of acute tonsillitis.footnote 1
Be safe with medicines. Read and follow all instructions on the label.
Tonsillitis caused by bacteria
Antibiotics are prescribed for tonsillitis caused by strep bacteria. A strep infection will usually go away on its own, but antibiotic treatment is needed because untreated strep throat can cause serious complications. For more information, see the topic Strep Throat.
If antibiotics are prescribed, be sure you take them exactly as directed by your doctor. Antibiotics should be taken for the entire duration of the prescription, even if the symptoms disappear completely before the prescription is gone. If antibiotics used to treat tonsillitis are not taken as directed, bacteria can become resistant to them (antibiotic resistance). In these cases, antibiotic treatment of future infections may not work.
Surgery
Surgical removal of the tonsils (tonsillectomy) is still a common procedure, particularly for children. But it is not done nearly as often as it was in the past. Tonsillectomy may be considered to treat tonsillitis when a child has serious complications, recurrent infections, or chronic infections that do not respond to treatment and interfere with daily functioning. But the risks and benefits of surgery need to be weighed carefully. Tonsillectomy should only be done after you and your doctor carefully consider your or your child’s overall health.
Prevention
A wide variety of viruses and bacteria can cause tonsillitis, so the best prevention is to follow basic health and hygiene precautions. These steps are especially helpful for children:
- Avoid close contact with others who are sick. If possible, keep your child away from children who are known to have tonsillitis or a sore throat.
- Often remind your child about the importance of proper hand-washing, especially when around people who appear to be sick. Also tell your child not to share toothbrushes or eating utensils with other children.
- Wash and disinfect surfaces and toys.
- Teach children to cover their mouths when coughing or sneezing, preferably using a tissue so that germs do not get on their hands. Also show them how to use tissues to wipe their noses.
- Carry disposable wipes and a hand sanitizer to clean hands and to wipe off shopping carts or other shared items in public places.
- Do not smoke around your child.
Home Treatment
The goal of home treatment of tonsillitis caused by a virus is to manage symptoms as the body fights off the infection. Home treatment eases the discomfort of sore throat and symptoms such as runny nose, nasal congestion, sneezing, and coughing.
Things that may help you or your child feel better include:
- Gargling often with warm salt water if your child is age 8 or older. You can make your own salt water by mixing 1 tsp (5 g) salt with 8 fl oz (240 mL) warm water.
- Drinking warm or cool liquids (whichever feels better). These include tea, soup, juice, and rehydration drinks.
- Eating flavored ice pops, such as Popsicles.
- Getting plenty of rest.
- Using a vaporizer or humidifier in the bedroom.
- Using throat lozenges to help relieve sore throat symptoms. But lozenges should not be given to young children because of the risk of choking. Also, many lozenges contain unneeded ingredients that can be potentially harmful.
Ask your doctor if you can take over-the-counter pain medicines (such as acetaminophen or ibuprofen) to help relieve sore throat pain. Be safe with medicines. Read and follow all instructions on the label. If you give medicine to your baby, follow your doctor’s advice about what amount to give. Do not give aspirin to anyone younger than 20 because of its link to Reye syndrome, a serious but rare problem.
Cough and cold medicines may not be safe for young children or for people who have certain health problems. Before you use these medicines, check the label. Many over-the-counter remedies, including antiseptic mouthwashes, decongestants, and antihistamines, contain extra ingredients that don’t relieve discomfort. These remedies are not recommended for children, as these ingredients have not been proved to have any benefits in the treatment of acute tonsillitis.footnote 1
A sore throat along with sudden fever and swollen lymph nodes, and without symptoms of an upper respiratory tract infection, may point to a bacterial infection. Anyone with these symptoms should see a doctor to be tested for strep throat, which requires treatment with antibiotics. It is important to get plenty of rest and take all the prescribed antibiotics exactly as directed. Keep your child home from school for the first 1 to 2 days of antibiotic treatment. He or she is still contagious during this time and might pass the infection to others.
Medications
Tonsillitis is usually caused by a virus and does not require prescription medicine. For information on over-the-counter pain medicine and other self-care options, see Home Treatment.
An antibiotic, usually amoxicillin or penicillin, is used to treat tonsillitis caused by strep bacteria. Although tonsillitis caused by strep bacteria usually will go away on its own, antibiotics are used to prevent the complications, such as rheumatic fever, that can result from untreated strep throat.
What to think about
If antibiotics are prescribed, be sure you take them exactly as directed by your doctor until the medicine is gone. Even if the symptoms go away completely before the prescription is gone, all pills should be taken as directed to make sure the infection is completely destroyed. Bacteria can become resistant to the antibiotics used to treat tonsillitis (antibiotic resistance) if prescriptions aren’t taken as directed or if they are prescribed when they aren’t needed.
Surgery
Tonsillectomy for tonsillitis is generally used for children who have serious complications or recurrent infections that do not respond to other treatment, especially when they interfere with daily life. But tonsillectomy should only be done after you and your doctor carefully consider your child’s medical history and overall health.
Researchers in a recent study concluded that tonsillectomy may be no better than watchful waiting for children who have mild symptoms, which was defined as tonsillitis occurring fewer than 3 times a year.footnote 2
But for some children, tonsillectomy can greatly improve their quality of life. Children who are most likely to benefit from tonsillectomy are those who have:
- 7 or more episodes of tonsillitis in 1 year, or 5 or more episodes a year for the past 2 years, or 3 or more episodes a year for the past 3 years. Tonsillectomy is more likely to be considered as treatment when some of these episodes result in missing school, trouble sleeping, or having other problems with normal daily life.footnote 2
- Tonsillitis lasting longer than 3 months, despite medicine.
- Obstructed air passages.
- Difficulty swallowing.
- Difficulty talking because of nasal obstruction.
- Tonsils that bleed heavily.
Surgery choices
Tonsillectomy for strep throat may be done in cases of recurring tonsillitis that do not respond to antibiotics or if an infection threatens the child’s well-being.
What to think about
Tonsillectomy is still the most common major surgical procedure done on children in the United States. But it is not done as often as it was in the past.
Upper respiratory infections and tonsillitis usually occur less frequently as a child gets older. Consider whether your child’s tonsillitis infections are manageable until you can wait to see if he or she outgrows them.
A child who has tonsillectomy will need special care and close monitoring for at least a week after the surgery. Consider your ability to provide this care for your child before deciding on tonsillectomy.
References
Citations
- Cherry JD (2009). Pharyngitis (pharyngitis, tonsillitis, tonsillopharyngitis, and nasopharyngitis). In RD Feigin et al., eds., Feigin and Cherry’s Textbook of Pediatric Infectious Diseases, 6th ed., vol. 2, pp. 160–169. Philadelphia: Saunders.
- Baugh RF, et al. (2011). Clinical practice guideline: Tonsillectomy in children. Otolaryngology–Head and Neck Surgery, 144(IS): S1–S30.
Other Works Consulted
- Georgalas CC, et al. (2014). Tonsillitis. BMJ Clinical Evidence. http://clinicalevidence.bmj.com/x/systematic-review/0503/overview.html. Accessed April 14, 2016.
- Isaacson G (2012). Tonsillectomy care for the pediatrician. Pediatrics, 130(2): 324–334.
- Simon HB (2006). Bacterial infections of the upper respiratory tract. In DC Dale, DD Federman, eds., ACP Medicine, section 7, chap. 19. New York: WebMD.
- Suurna MV (2012). Management of adenotonsillar disease. In AK Lalwani, ed., Current Diagnosis and Treatment: Otolaryngology—Head and Neck Surgery, 3rd ed., pp. 362–368. New York: McGraw-Hill.
- Wetmore RF (2011). Tonsils and adenoids. In RM Kliegman et al., eds., Nelson Textbook of Pediatrics, 19th ed., pp. 1442–1445. Philadelphia: Saunders.
Current as of: October 21, 2018
Author: Healthwise Staff
Medical Review:Adam Husney, MD – Family Medicine & John Pope, MD, MPH – Pediatrics & E. Gregory Thompson, MD – Internal Medicine & Kathleen Romito, MD – Family Medicine & Charles M. Myer III, MD – Pediatrics, Otolaryngology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.