Type 1 Diabetes: Children Living With the Disease
Topic Overview
Is this topic for you?
This topic covers type 1 diabetes in children. For information about type 1 diabetes in adults and about preventing complications from type 1 diabetes, see the topic Type 1 Diabetes.
What is type 1 diabetes?
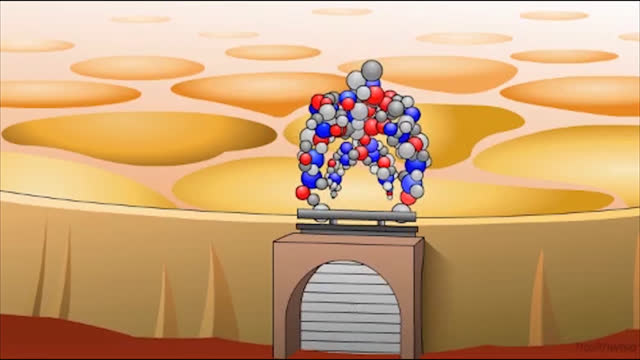
Type 1 diabetes develops when the pancreas stops making insulin. Your body needs insulin to let sugar (glucose) move from the blood into the body’s cells, where it can be used for energy or stored for later use.
Without insulin, the sugar cannot get into the cells to do its work. It stays in the blood instead. This can cause high blood sugar levels. A person has diabetes when the blood sugar is too high.
What will it be like for your child to live with type 1 diabetes?
Your child can live a long, healthy life by learning to manage his or her diabetes. It will become a big part of your and your child’s life.
You play a major role in helping your child take charge of his or her diabetes care. Let your child do as much of the care as possible. At the same time, give your child the support and guidance he or she needs.
How can you manage diabetes?
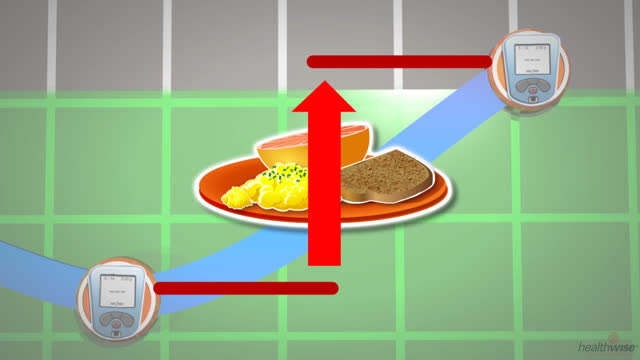
The key to managing diabetes is to keep blood sugar levels in a target range. To do this, your child needs to take insulin, eat about the same amount of carbohydrate at each meal, and exercise. Part of your child’s daily routine also includes checking his or her blood sugar levels at certain times, as advised by your doctor.
The longer a person has diabetes, the more likely he or she is to have problems, such as diseases of the eyes, heart, blood vessels, nerves, and kidneys. For some reason, children seem protected from these problems during childhood. But if your child can control his or her blood sugar levels every day, it may help prevent problems later on.
What symptoms should you watch for?
Even when you are careful and do all the right things, your child can have problems with low or high blood sugar. Teach your child to look for signs of low and high blood sugar and to know what to do if this happens.
- If your child has low blood sugar, he or she may sweat a lot and feel weak, shaky, or hungry. But your child’s symptoms may be different. Low blood sugar happens quickly. A person can get low blood sugar within minutes after exercise or after taking insulin without eating enough.
- If your child has high blood sugar, he or she may be very thirsty or hungry, have to urinate more often than usual, or have blurry vision. High blood sugar usually develops slowly over hours or days.
Young children can’t tell if they have low blood sugar as well as adults can. Also, after your child has had diabetes for a long time, he or she may not notice low blood sugar symptoms anymore. This raises the chance that your child could have low blood sugar emergencies. If you are worried about your child’s blood sugar, do a home blood sugar test. Don’t rely on symptoms alone.
Both low and high blood sugar can cause problems and need to be treated. Your doctor will suggest how often your child’s blood sugar should be checked.
How often does your child need to see the doctor?
See your child’s doctor at least every 3 to 6 months to check how well the treatment is working. During these visits, the doctor will do some tests to see if your child’s blood sugar is under control. Based on these results, the doctor may change your child’s treatment plan.
When your child is 10 years old or starts puberty, he or she will start having exams and tests to look for any problems from diabetes.
How will your child’s treatment change over time?
Your child’s insulin dose and possibly the types of insulin may change over time. The way your child takes insulin (with shots or an insulin pump) also may change. This is especially true during the teen years when your child grows and changes a lot.
What and how much food your child needs will also change over the years. But it will always be important to eat about the same amount of carbohydrate at each meal. Carbohydrate is the nutrient that most affects blood sugar.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
- Diabetes in Children: Checking Blood Sugar in a Child
- Diabetes in Children: Giving Insulin Shots to a Child
- Diabetes in Children: Preparing a Care Plan for School
- Diabetes in Children: Preventing High Blood Sugar
- Diabetes in Children: Treating Low Blood Sugar
- Diabetes: Counting Carbs if You Use Insulin
- Diabetes: Living With an Insulin Pump
Cause
Type 1 diabetes develops because the body’s immune system destroys beta cells in a part of the pancreas called the islet tissue. Beta cells produce insulin. So children with type 1 diabetes can’t make their own insulin. Experts do not know what causes this to happen. But the cause may involve family history and maybe environmental factors like diet or infections.
Type 1 diabetes develops when your child’s pancreas stops producing enough insulin. Insulin lets blood sugar—also called glucose—enter the body’s cells, where it is used for energy. Without insulin, the amount of sugar in the blood rises above a safe level. As a result, your child experiences high and low blood sugar levels from time to time. High blood sugar can damage blood vessels and nerves throughout the body and increases your child’s risk of eye, kidney, heart, blood vessel, and nerve diseases.
Causes of high blood sugar
- Not getting enough insulin or eating more than usual
- Experiencing emotional stress
- Having an illness, such as the flu or an infection
- Taking certain medicines that can raise blood sugar levels, such as medicines that reduce swelling and inflammation (corticosteroids) and growth hormone
- Experiencing the dawn phenomenon or the Somogyi effect, which causes high blood sugar in the morning
- Entering puberty. Hormonal changes affect how well the body uses insulin. These changes can cause higher blood sugar levels.
- Pregnancy
Causes of low blood sugar
- Taking too much insulin
- Skipping or delaying a meal or snack
- Being more physically active than usual without eating enough food
- Taking certain medicines that may lower blood sugar levels, such as those that reduce fever and pain
- Starting your menstrual period, because hormonal changes may affect how well insulin works
Symptoms
Because your child has type 1 diabetes, he or she will experience high and low blood sugar levels from time to time. High blood sugar usually develops slowly over hours or days, so you can treat the symptoms before they become severe and require medical attention. On the other hand, your child’s blood sugar level can drop to dangerously low levels in minutes.
Be alert for:
- Symptoms of low blood sugar, which include sweating, weakness, and hunger.
- Symptoms of high blood sugar, which include increased thirst and increased urination.
How can you tell the difference?
Sometimes it’s hard to distinguish between high and low blood sugar symptoms, especially if your child is very young. Test your child’s blood sugar whenever you think it may be high or low so that you can treat it appropriately. If your child has symptoms of very high blood sugar, such as a fruity breath odor, vomiting, and/or belly pain, seek emergency care. These symptoms may point to diabetic ketoacidosis, which is a life-threatening emergency.
What Happens
Every child experiences type 1 diabetes differently.
The negative effects of diabetes are caused by blood sugar levels that are above or below a target range.
Low blood sugar
Very low blood sugar is a frightening experience for you and your child. But if low blood sugar levels are treated quickly and appropriately, your child should have no lasting effects.
Young children cannot recognize low blood sugar symptoms as well as adults can, which puts them at risk for low blood sugar emergencies. Children who develop hypoglycemia unawareness, which is the inability to recognize early symptoms of low blood sugar until they become severe, or who are trying to keep their blood sugar levels tightly within a target range are also at risk for low blood sugar emergencies.
Make sure your child’s caregivers, such as school nurses, know:
- How to watch for symptoms of low blood sugar.
- How to do a home blood sugar test.
- What to do if your child’s blood sugar level is low, such as knowing how to give glucagon.
Let your doctor know if your child is having frequent episodes of low blood sugar. You can use this form( What is a PDF document? ) to keep a record of your child’s very high or very low blood sugar levels.
High blood sugar
Very high blood sugar puts your child at risk for diabetic ketoacidosis, a life-threatening emergency. Skipping insulin injections, stress, illness, injury, and puberty can trigger high blood sugar. Because blood sugar levels usually rise slowly, you can treat symptoms early and, most often, prevent diabetic ketoacidosis.
High blood sugar can also lead to:
- Adjustment of the body to high levels. For example, if your child’s blood sugar level is consistently at 250 milligrams per deciliter (mg/dL) and suddenly drops to 100 mg/dL, you or your child may think this level is too low when it is really not. Your child may even have symptoms of low blood sugar at target blood sugar levels.
- Delayed growth and maturity. If your child has high blood sugar levels over a long period of time, he or she may grow and mature more slowly. During puberty, this can delay normal sexual development and the onset of menstruation. And your child may not gain weight properly if he or she doesn’t have enough insulin.
- Complications from the disease (eye, kidney, heart, blood vessel, and nerve disease). But if their blood sugar levels are persistently high, children are more likely to show early signs of these problems, particularly eye and kidney disease. Also, high blood sugar levels during childhood and adolescence put your child at risk for these diseases in early adulthood.
What can be done?
The best way to help your child with type 1 diabetes live a long and healthy life is to keep his or her blood sugar levels within a target range. Work with your child’s doctor, and monitor blood sugar levels frequently.
What Increases Your Risk
Risk factors for very high or low blood sugar levels in a child with type 1 diabetes include:
- Age. Very young children are at the greatest risk for very low blood sugar, because they are often not able to communicate symptoms.
- Tight blood sugar control. Although keeping your child’s blood sugar levels tightly within a target range is important, this puts him or her at risk for frequent low blood sugar levels.
- Persistent high blood sugar levels. Children who have persistent high blood sugar, indicated by higher hemoglobin A1c test results, are at greater risk for diabetic ketoacidosis than children who have lower levels.
- Puberty. Growth spurts and changing hormone levels that occur during puberty make it difficult to keep a child’s blood sugar level within a target range.
- Psychiatric conditions. Children with depression, anxiety disorder, panic disorder, or eating disorders are at increased risk for frequent high and low blood sugar levels.
When should you call your doctor?
Call 911 or other emergency services right away if your child:
- Has symptoms of diabetic ketoacidosis (DKA), such as:
- Blurred vision.
- Trouble staying awake or trouble being woken up.
- Fast, deep breathing.
- Breath that smells fruity.
- Belly pain, not feeling hungry, and vomiting.
- Feeling confused.
- Has passed out (lost consciousness) or has suddenly become very sleepy or confused. (Your child may have very low blood sugar, called hypoglycemia.)
Call a doctor if your child:
- Is sick and has blood sugar that cannot be controlled.
- Has been vomiting or has had diarrhea for more than 6 hours.
- Has blood sugar that stays higher than the level the doctor has set for your child, for example, 240 mg/dL for two or more readings.
- Has blood sugar that stays lower than the level the doctor has set for your child, for example, 70 mg/dL for two or more readings.
- Has symptoms of low blood sugar, such as:
- Sweating.
- Feeling nervous, shaky, and weak.
- Extreme hunger and slight nausea.
- Dizziness and headache.
- Blurred vision.
- Confusion.
Check with your doctor if your child:
- Often has problems with high or low blood sugar levels.
- Has trouble knowing when his or her blood sugar is low (hypoglycemia unawareness).
- Or you have questions or want to know more about diabetes.
Who to see
Health professionals who may care for a child who has with type 1 diabetes include:
- A pediatrician, a family medicine doctor, or a general practitioner.
- A nurse practitioner or a physician assistant.
- A pediatric endocrinologist.
- A certified diabetes educator (CDE).
- A registered dietitian, to help develop a daily meal plan for your child and your family.
- A psychologist, to help with emotional or family issues that might affect your child’s treatment.
Exams and Tests
A child with type 1 diabetes needs to visit his or her doctor at least every 3 to 6 months. During these visits, the doctor reviews your child’s blood sugar level records and asks about any problems you and your child may have. Your child’s blood pressure is checked, and growth and development is evaluated. The doctor examines your child for signs of infections, especially at injection sites. Your child usually has the following tests at office visits:
- A hemoglobin A1c or similar test (glycosylated hemoglobin or glycohemoglobin) to check your child’s blood sugar control over the previous 3 months
- A blood glucose test
If your child is at least 10 years old, your child’s doctor may do a cholesterol (LDL and HDL) test when type 1 diabetes is diagnosed or as soon as blood sugars are under control. If the LDL cholesterol is less than 100 mg/dL (2.60 mmol/L), the doctor may repeat this test every 3 to 5 years.
Diabetes increases your child’s risk for dental problems. Experts suggest dental checkups every 6 months.
Once a year, you and your child may also see other members of the diabetes team, for example:
- A certified diabetes educator or registered dietitian, for your child’s changing nutritional needs.
- A social worker, for questions about insurance.
- A psychologist, to help with any emotional or behavioral issues.
5 years after diagnosis
Your child will have an initial dilated eye exam (ophthalmoscopy) by an ophthalmologist or an optometrist if your child has had diabetes for 3 to 5 years and has started puberty or has had diabetes for 3 to 5 years and is at least 10 years old. This eye exam checks for signs of diabetic retinopathy and glaucoma. Thereafter, your child may have an eye exam every year. If your child is at low risk for vision problems, your doctor may consider follow-up exams less often.
Your child’s doctor will also start doing an annual urine test to check for protein. This test helps detect diabetic nephropathy.
Other tests
Your child may have a test for thyroid antibodies when type 1 diabetes is diagnosed. Also, a thyroid-stimulating hormone (TSH) test and a thyroxine (T4) test may be done every 1 to 2 years. These tests check for thyroid problems, which are common among people who have type 1 diabetes.
Some other tests include:
- Annual foot exam if your child has had diabetes for 5 years and has started puberty or has had diabetes for 5 years and is at least 10 years old.
- Routine screening for depression after your child is 10 years old.
- Eating disorder evaluation if your child shows signs of an eating problem.
- Celiac disease testing when type 1 diabetes is diagnosed and then if your child is not growing or gaining weight as much as expected.
Treatment Overview
The goal of your child’s treatment for type 1 diabetes is to always keep his or her blood sugar levels within a target range. A target range reduces the chance of diabetes complications. Daily diabetes care and regular medical checkups will help you and your child accomplish this goal.
Daily care
Your child’s daily care includes:
- Exercise. Experts recommend that teens and children (starting at age 6) do moderate to vigorous activity at least 1 hour every day.footnote 1
- Home blood sugar monitoring.
- Preparing and giving insulin injections.
- Living with an insulin pump.
- Counting carbohydrate.
- Dealing with low blood sugar levels.
- Preventing high blood sugar levels.
Some problems you may encounter include:
- Changing appetite and “picky eating.” A registered dietitian can help you build a flexible meal plan to meet your child’s appetite needs and allow for special events, such as parties and school activities. If you use rapid-acting insulin, you can give the insulin dose after a meal based on what your child ate. Some tips for mealtimes with young children include having alternative meal choices.
- Illness. Work with your doctor to set up sick-day guidelines for your child. These help you prevent high blood sugar emergencies when your child is ill. Talk with the doctor before giving your child any nonprescription medicine.
- Exercise. Plan some activities to do with your child, such as in-line skating or bicycling. Use these tips for exercising safely to help prevent low blood sugar in your child. Limit TV, video games, and computer time.
You will also want to:
- Always have your child wear medical identification to let medical personnel know that he or she has diabetes. You can buy medical identification bracelets, necklaces, or other forms of jewelry at a pharmacy or on the Internet. Temporary medical identification tattoos are another form of medical identification.
- Teach your child about good foot care. Foot problems are rare in children who have diabetes. But adults can have foot problems, especially with diabetic neuropathy. Teach your child the importance of wearing shoes that fit properly. Check your child’s feet if he or she has signs of injury or infection. Teach your child to get in the habit of washing and drying feet thoroughly. If you notice a foot problem, even a minor one, talk with your child’s doctor before treating it.
- Keep your child’s day care or school plan for diabetes care up to date. Have written instructions for your babysitter and other caregivers.
- Help your child care for his or her skin and teeth and gums. Make sure your child has a dental checkup every 6 months.
- Keep your child’s immunizations up to date. This includes a flu shot every year.
- Participate in a support group for parents of children who have diabetes. These groups can be very helpful, especially the first few years after diagnosis. Local groups are available in most areas.
- Encourage your child to attend camps for children who have diabetes. Diabetes camps are a good learning experience for your child, and they will allow you some time to yourself.
- Allow your child who has diabetes to help with the treatment, given his or her age and experience with the disease.
Regular medical checkups
Your child needs to see his or her doctor every 3 to 6 months. During these checkups, the doctor will evaluate and adjust your child’s treatment. The doctor will do a hemoglobin A1c or similar test (glycosylated hemoglobin or glycohemoglobin) to check your child’s blood sugar control over the previous 2 to 3 months, and a blood glucose test.
If your child’s LDL cholesterol is less than 100 mg/dL (2.60 mmol/L) and there is no family history of high cholesterol, the doctor may do a cholesterol (LDL and HDL) test every 5 years. If your child’s blood pressure is consistently high and not reduced with weight control or exercise, the doctor may consider medicine.
When your child has had diabetes for 5 years, the doctor will start yearly screening tests for protein in the urine, which points to diabetic nephropathy. At that same time, your child needs to see an ophthalmologist for yearly dilated eye exams (ophthalmoscopy) to check for signs of diabetic retinopathy. If your child is at low risk for vision problems, your doctor may consider doing follow-up exams less often.
Treatment for high blood sugar emergency
If your child does not take enough insulin, has a severe infection or other illness, or becomes severely dehydrated, his or her blood sugar level may rise very high and lead to diabetic ketoacidosis. Diabetic ketoacidosis is almost always treated in a hospital, often in the intensive care unit, where caregivers can watch your child closely and give him or her frequent blood tests for glucose and electrolytes. Insulin is given through a vein (intravenous, or IV) to bring blood sugar levels down. Fluids are given through the IV to correct the electrolyte imbalance. Your child may stay in the hospital for a few days until blood sugar levels are back in the target range and electrolytes have normalized.
What to think about
For some children, using an insulin pump may help keep their blood sugar levels within a target range.
If your child has frequent low blood sugar levels, especially at night (nocturnal hypoglycemia), the doctor may suggest a continuous glucose monitor (CGM). A CGM checks and records blood sugar day and night. Most CGMs sound an alarm if blood sugar levels are moving out of target range.
Prevention
Your child with type 1 diabetes will have high and low blood sugar levels from time to time. You can help avoid many immediate problems and long-term complications, such as eye, kidney, heart, blood vessel, and nerve disease, by:
- Helping your child develop a healthy attitude toward having diabetes. As your child grows and develops, let him or her assume appropriate responsibility for treatment.
- Encouraging and supporting your child to keep blood sugar levels within a target range. Starting tight control of blood sugar levels as soon as possible after diagnosis of diabetes gives your child the greatest chance of avoiding complications from diabetes later on in life.
- Checking your child’s blood sugar level several times a day and whenever you think it may be high or low.
- Recognizing and treating high and low blood sugar quickly. Make sure everyone who cares for your child knows how to treat high and low blood sugar episodes.
- Discussing the dangers of smoking, drinking alcohol, and using other drugs. Smoking affects the blood vessels and can lead to diabetes complications. Alcohol and other drugs may cause low blood sugar and can mask symptoms of low blood sugar, which may lead to an emergency situation.
- Keeping your child’s immunizations up to date. Diabetes affects the immune system, increasing the risk of developing a severe illness.
- Keeping your child’s doctor aware of behavior changes in your child. Emotions and behavior can affect how well you and your child manage diabetes treatment.
Medications
Insulin is the only medicine that can treat type 1 diabetes, and your child is most likely taking more than one type of insulin. Your child may take several injections a day or use an insulin pump. The insulin pump provides insulin with fewer injections and is as effective as multiple daily injections for keeping blood sugar levels in a target range.
The amount and type of insulin your child takes will likely change over time, depending on changes that occur with normal growth, physical activity level, and hormones (such as during adolescence). Your child may also need higher doses of insulin when feeling sick or stressed.
- Know what the dose is for each type of insulin your child takes, when your child should take the doses, how long it takes for each type of insulin to start working (onset), when it will have its greatest effect (peak), and how long it will work (duration).
- Store insulin bottles and insulin in pens or pumps according to the manufacturer’s instructions. Insulin exposed to heat and sunlight can be less effective.
- Don’t let your child skip a dose of insulin without a doctor’s advice.
What to think about
A rapid-acting insulin is given with a meal or immediately afterward. The dose is based on what your child actually ate, not what the meal plan required. If your child is a “picky eater,” this provides flexibility that may reduce mealtime battles.
Scientists are looking at new types of insulin and better ways to give it.
Other Treatment
Other types of meal plans
You may hear of people with diabetes following other types of meal plans or using low glycemic index foods to prevent high blood sugar levels after meals. Talk with a registered dietitian before trying a new meal plan.
Complementary therapies
Along with medical treatment, you may wonder if complementary therapies, especially dietary supplements, will help your child. There isn’t enough scientific evidence to say that any dietary supplement can prevent or manage type 1 diabetes.footnote 2
Talk with your doctor about any complementary health practice that you would like your child to try or that your child is already using. Your doctor can help you manage your child’s health better if he or she knows about all of your child’s health practices.
References
Citations
- U.S. Department of Health and Human Services (2008). 2008 Physical Activity Guidelines for Americans (ODPHP Publication No. U0036). Washington, DC: U.S. Government Printing Office. Available online: http://www.health.gov/paguidelines/guidelines/default.aspx.
- National Center for Complementary and Integrative Health (2008, updated 2014). Diabetes and dietary supplements: In depth. National Center for Complementary and Integrative Health. https://nccih.nih.gov/health/diabetes/supplements.
Other Works Consulted
- American Diabetes Association (2017). Standards of medical care in diabetes—2017. Diabetes Care, 40(Suppl 1): S1–S135.
- Alemzadeh R, Ali O (2011). Diabetes mellitus. In RM Kliegman et al., eds., Nelson Textbook of Pediatrics, 19th ed., pp. 1968–1997. Philadelphia: Saunders.
- American Diabetes Association (2012). Diabetes care for emerging adults: Recommendations for transition from pediatric to adult diabetes care systems. Diabetes Care, 34(11): 2477–2485.
- American Diabetes Association (2012). Diabetes management at camps for children with diabetes. Diabetes Care, 35(Suppl 1): S72–S75.
- Beaser RS (2010). Designing a conventional insulin treatment program. In RS Beaser, ed., Joslin’s Diabetes Deskbook: A Guide for Primary Care Providers, 2nd ed., pp. 297–340. Boston: Joslin Diabetes Center.
- Campbell AP, Beaser RS (2010). Medical nutrition therapy. In RS Beaser, ed., Joslin’s Diabetes Deskbook: A Guide for Primary Care Providers, 2nd ed., pp. 91–136. Boston: Joslin Diabetes Center.
- Jackson CC, et al. (2015). Diabetes care in the school setting: A position statement of the American Diabetes Association. Diabetes Care, 38(1): 1958–1963. DOI: 10.2337/dc15-1418. Accessed January 11, 2016.
- Pignone M, et al. (2010). Aspirin for primary prevention of cardiovascular events in people with diabetes: A position statement of the American Diabetes Association, a scientific statement of the American Heart Association, and an expert consensus document of the American College of Cardiology Foundation. Circulation, 121(24): 2694–2701.
- Rewers M, et al. (2014). Diabetes mellitus. In WW Hay et al., eds., Current Diagnosis and Treatment: Pediatrics, 22nd ed., pp. 1097–1105. New York: McGraw-Hill.
- Rosenbloom AL (2011). Diabetes mellitus. In CD Rudolph et al., eds., Rudolph’s Pediatrics, 22nd ed., pp. 2104–2125. New York: McGraw-Hill.
- Siminerio LM, et al. (2014). Care of young children with diabetes in the child care setting: A position statement of the American Diabetes Association. Diabetes Care, 37(10): 2834–2842. DOI: 10.2337/dc14-1676. Accessed October 9. 2014.
- Wolfsdorf J, et al. (2006). Diabetic ketoacidosis in infants, children, and adolescents: A consensus statement from the American Diabetes Association. Diabetes Care (29): 1150–1159.
Current as of: April 16, 2019
Author: Healthwise Staff
Medical Review:John Pope MD – Pediatrics & Kathleen Romito MD – Family Medicine & Adam Husney MD – Family Medicine & Stephen LaFranchi MD – Pediatrics, Pediatric Endocrinology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.