Guillain-Barré Syndrome
Topic Overview
What is Guillain-Barré syndrome?
Guillain-Barré syndrome (say “ghee-YAN bah-RAY”) is a problem with your nervous system. It causes muscle weakness, loss of reflexes, and numbness or tingling in your arms, legs, face, and other parts of your body.
This rare condition can cause paralysis and lead to death. But most people get better and have few lasting problems.
What causes Guillain-Barré syndrome?
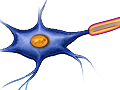
Experts don’t know what causes it. They think that the nerves are attacked by your body’s own defense system (the immune system). This is called an autoimmune disease.
In Guillain-Barré syndrome, the immune system attacks the covering (myelin sheath) of certain nerves. This causes nerve damage.
Infections that may trigger Guillain-Barré syndrome
It usually begins to affect the nerves after you’ve had a viral or bacterial infection. Often it is after an infection of the lungs or stomach and intestines.
Infections that may trigger it include:
- Campylobacter jejuni, which can cause a type of food poisoning.
- Cytomegalovirus (CMV), which can cause fever, chills, sore throat, swollen glands, body aches, and fatigue.
- Epstein-Barr virus (EBV), which can cause mononucleosis (mono).
- Human immunodeficiency virus (HIV), which can cause fatigue, weight loss, fever, night sweats, diarrhea, and other symptoms.
- Mycoplasma, which can cause pneumonia.
- Varicella-zoster virus, which can cause chickenpox and shingles.
- Zika virus, which can cause fever, rash, painful joints, and red eyes.
What are the symptoms?
Symptoms include:
- Numbness or tingling in your hands and feet and sometimes around the mouth and lips.
- Muscle weakness in your legs and arms and the sides of your face.
- Trouble speaking, chewing, and swallowing.
- Not being able to move your eyes.
- Back pain.
Symptoms usually start with numbness or tingling in the fingers and toes. Over several days, muscle weakness in the legs and arms develops. After about 4 weeks, most people begin to get better.
You may need to be treated in the hospital for the first few weeks. This is because the condition can be deadly if weakness spreads to muscles that control breathing, heart rate, and blood pressure.
Call your doctor or get help right away if you think you might have Guillain-Barré syndrome.
How is Guillain-Barré syndrome diagnosed?
Your doctor will ask when your symptoms started and how they have changed. He or she also may ask if you’ve had any recent infections.
Two signs are important in helping your doctor decide if you have Guillain-Barré syndrome:
- Your arms and legs are getting weaker.
- You are losing your reflexes, which are automatic body movements that you can’t control.
Your doctor also may do tests, such as a lumbar puncture and a nerve conduction study.
If the diagnosis isn’t clear, you may be referred to a doctor who specializes in the nervous system (neurologist).
How is it treated?
This syndrome usually is treated in the hospital. The hospital staff will watch you carefully to be sure you don’t get worse or get an infection. Your breathing, heart rate, and blood pressure are carefully tracked. Some people need a ventilator to help them breathe.
In the hospital, you may get a plasma exchange or intravenous immune globulin (IVIG).
- In a plasma exchange, blood is taken out of your body. The harmful antibodies are removed from the blood, and then the blood is returned to your body.
- In IVIG, helpful antibodies are added to your blood.
These treatments may help your body fight the disease and may speed your recovery if they are used when you first get sick. You may need to stay in the hospital for weeks or longer, until your symptoms have improved.
Sometimes this condition can come back. Both plasma exchange and IVIG therapy may be needed to reduce the severity of a relapse.
How long will it take to recover?
You may need 3 to 6 months or longer to recover. And you may have to wait several months before you can return to your regular activities.
Many people have long-term effects, such as numbness in the toes and fingers. In most cases, these problems won’t get in the way of your daily life. Some people have more serious problems, such as long-term weakness or balance problems.
Support at home is important during this time. You may need some help with some of your activities and chores until you’re stronger.
Regular exercise can help you strengthen your weakened muscles. Talk to your doctor about exercising during your recovery. If you have severe muscle weakness, you may need physical or occupational therapy.
References
Other Works Consulted
- Brannagan TH, Weimer LH (2010). Acquired neuropathies. In LP Rowland, TA Pedley, eds., Merritt’s Neurology, 12th ed., pp. 822–837. Philadelphia: Lippincott Williams and Wilkins.
- Cortese I, et al. (2011). Evidence-based guideline update: Plasmapheresis in neurologic disorders: Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology, 76(3): 294–300.
- Hughes RAC, et al. (2003, reaffirmed 2008). Practice parameter: Immunotherapy for Guillain-Barré syndrome. Neurology, 61(6): 736–740.
- Hughes RAC, et al. (2012). Intravenous immunoglobulin for Guillain-Barré syndrome. Cochrane Database of Systematic Reviews (7).
- Patwa HW, et al. (2012). Evidence-based guideline: Intravenous immunoglobulin in the treatment of neuromuscular disorders. Neurology, 78(13): 1009–1015.
- Raphaël JC (2012). Plasma exchange for Guillain-Barré syndrome. Cochrane Database of Systematic Reviews (7).
- Ropper AH, et al. (2014). Diseases of the peripheral nerves. In Adams and Victor’s Principles of Neurology, 10th ed., pp. 1310–1390. York: McGraw-Hill Education.
Credits
Current as ofMarch 28, 2019
Author: Healthwise Staff
Medical Review: Anne C. Poinier, MD – Internal Medicine
E. Gregory Thompson, MD – Internal Medicine
Adam Husney, MD – Family Medicine
Martin J. Gabica, MD – Family Medicine
Kathleen Romito, MD – Family Medicine
Colin H. Chalk, MD, CM, FRCPC – Neurology
Current as of: March 28, 2019
Author: Healthwise Staff
Medical Review:Anne C. Poinier, MD – Internal Medicine & E. Gregory Thompson, MD – Internal Medicine & Adam Husney, MD – Family Medicine & Martin J. Gabica, MD – Family Medicine & Kathleen Romito, MD – Family Medicine & Colin H. Chalk, MD, CM, FRCPC – Neurology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.