Knee Replacement Surgery
Surgery Overview
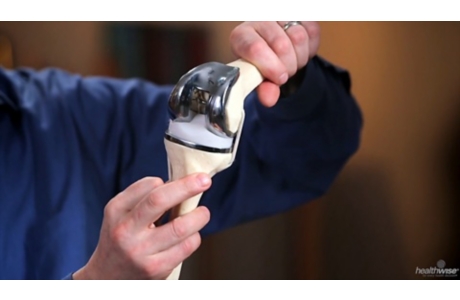
Joint replacement involves surgery to replace the ends of bones in a damaged joint. This surgery creates new joint surfaces.
In knee replacement surgery, the ends of the damaged thigh and lower leg (shin) bones and usually the kneecap are capped with artificial surfaces. These surfaces are lined with metal and plastic. In most cases, doctors replace the entire surface at the ends of the thigh and lower leg bones. Doctors usually secure knee joint components to the bones with cement.
Doctors are working on ways to replace just the damaged parts of the knee joint. This is sometimes called partial joint replacement. Unicompartmental replacement is one example of partial knee replacement. It replaces just the inner knee surfaces or the outer knee surfaces, depending on where the damage is. Another partial replacement is called a patellofemoral replacement. In this surgery, the end of the thigh bone is replaced. Then an artificial surface is used to line the back of the kneecap.
In knee replacement surgery, doctors remove the damaged cartilage and replace it with new joint surfaces in a step-by-step process.
Joint changes caused by osteoarthritis may also stretch and damage the ligaments that connect the thighbone to the lower leg bone. After surgery, the artificial joint itself and the remaining ligaments around the joint usually provide enough stability so that the damaged ligaments are not a problem.
Your doctor may use general anesthesia. This means you’ll be asleep during the surgery. But sometimes doctors use regional anesthesia. This means you can’t feel the area of the surgery. You will feel sleepy, but you will be awake. Which type of anesthesia you get depends on your doctor and on your overall health. Your doctor might also ask what you prefer.
Your doctor may recommend that you take antibiotics before and after the surgery to reduce the risk of infection. If you need any major dental work, your doctor may recommend that you have it done before the surgery. Infections can spread from other parts of the body, such as the mouth, to the artificial joint and cause a serious problem.
What To Expect
Right after surgery
You will have intravenous (IV) antibiotics for about a day after surgery. You will also receive medicines to control pain, and perhaps medicines to prevent blood clots. It is not unusual to have an upset stomach or feel constipated after surgery. Talk with your doctor or nurse if you don’t feel well.
When you wake up from surgery, you will have a bandage on your knee. You will probably have a drain to collect fluid and keep it from building up around your joint. You may have a catheter. This is a small tube connected to your bladder so you don’t have to get out of bed to urinate. You may also have a compression pump or compression stocking on your leg. This device squeezes your leg. It keeps the blood circulating and helps prevent blood clots.
Your doctor may teach you to do simple breathing exercises to help prevent congestion in your lungs while your activity level is reduced. You may also learn to move your feet up and down to flex your muscles and keep your blood circulating.
The first few days
You will probably still take some medicine. Over time, you will take less and less pain medicine. You may keep taking medicines to prevent blood clots for at least 10 days after surgery.
Most people who have knee replacement surgery start to walk with a walker or crutches the day of surgery or the next day. And most people can bear weight on the knee if it is comfortable.
A physical therapist will help you gently bend and straighten your knee. Your therapist will also begin some simple exercises to help strengthen your leg muscles.
Rehabilitation (rehab) after a knee replacement is intensive. The main goal of rehab is to allow you to bend your knee at least 90 degrees. That much bend is enough for you to do daily activities, such as walk, climb stairs, sit in and get up from chairs, and get in and out of a car. Most people can bend the knee more than 90 degrees after surgery. But one of the things that affects how much bend you get after surgery is how much bend you had before surgery. To get the most benefit from your surgery, it is very important that you take part in physical therapy. You will get this therapy both while you are in the hospital and after you go home.
Your doctor will let you know if you will stay in the hospital or if you can go home the day of surgery. Some people who need more extensive rehab may go to a specialized rehab center for more treatment.
Continued recovery
After you go home, watch the surgery site and your general health. If you notice any redness or drainage from your wound, tell your surgeon. You may also be advised to take your temperature twice each day and to let your surgeon know if you have a fever over 100.5°F (38.1°C).
Rehab continues after you go home from the hospital. You will get rehab until you are able to function on your own and you get back as much strength and range of motion in your knee as you can. You will keep working on increasing the amount you can bend your knee and on building strength and endurance. Total rehab after surgery will take several months.
You will have an exercise program to follow when you go home, even if you are still having physical therapy. You should also take a short walk several times each day. If you notice any soreness, try a cold pack on your knee. You might also cut back on your activity a bit. But don’t stop completely. Staying on your walking and exercise program will help you recover faster.
Your doctor may recommend that you ride a stationary bike. It can help strengthen your leg muscles and improve your knee bending. Swimming is also a good exercise after knee surgery. But don’t go in the water until your stitches or staples are removed.
Living with a knee replacement
Your doctor may want to see you from time to time for several months or more to monitor your knee replacement. Over time, you will be able to do most of the things you could do before surgery.
Controlling your weight will help your new knee joint last longer.
Stay active to help keep your strength, flexibility, and endurance. Your activities might include walking, swimming (after your wound is completely healed), dancing, or golf. (If you golf, don’t wear shoes with spikes. And make sure to use a golf cart.) You could also try cycling on a stationary bike or on level surfaces.
For at least 2 years after your surgery, your doctor may want you to take antibiotics before dental work or any invasive medical procedure. This is to help prevent infection around your knee replacement. After 2 years, your doctor and dentist will decide whether you still need to take antibiotics. Your general health and the state of your other health conditions will help them decide.
Why It Is Done
Doctors recommend joint replacement surgery when knee pain and loss of function become severe and when medicines and other treatments no longer relieve pain. Your doctor will use X-rays to look at the bones and cartilage in your knee to see if they are damaged. This helps the doctor make sure that the pain isn’t coming from somewhere else.
Doctors may not recommend knee replacement for people who:
- Have poor general health and may not tolerate anesthesia and surgery well.
- Have an active infection or are at risk for infection.
- Have osteoporosis (significant thinning of the bones).
- Have severe weakness of the quadriceps muscles at the front of the thigh.
- Have a knee that appears to bend backward when the knee is fully extended (genu recurvatum), if this condition is due to muscle weakness or paralysis.
- Are severely overweight. Replacement joints may be more likely to fail in people who are very overweight.
Some doctors will recommend other types of surgery if possible for younger people and especially for those who do strenuous work. A younger or more active person is more likely than an older or less active person to have an artificial knee joint wear out. People who are very overweight are also more likely to have an artificial knee joint wear out from the extra stress on the joint.
Doctors usually don’t recommend knee replacement surgery for people who have very high expectations for how much they will be able to do with the artificial joint. (Examples are people who expect to be able to run, ski, or do other activities that stress the knee joint). The artificial knee allows a person to do ordinary daily activities with less pain. It does not restore the same level of function that the person had before the damage to the knee joint began.
How Well It Works
Most people have much less pain after knee replacement surgery and are able to do many of their daily activities more easily.
- The knee will not bend as far as it did before you developed knee problems. But the surgery will allow you to stand and walk for longer periods without pain.
- After surgery, you may be allowed to resume activities such as golfing, riding a bike, swimming, walking for exercise, dancing, or cross-country skiing (if you did these activities before surgery).
- Your doctor may discourage you from running, playing tennis, squatting, and doing other things that put a lot of stress on the joint.
The younger you are when you have the surgery and the more stress you put on the joint, the more likely it is that you will later need a second surgery to replace the first artificial joint. Over time, the components wear down or may loosen and need to be replaced.
Your artificial joint should last longer if you are not overweight and you do not do hard physical work or play sports that stress the joint.
People who have a partial knee replacement may have less pain. But in one study they were not as satisfied as people who had a total knee replacement.footnote 1
If you wait to have surgery until you have already lost a lot of your strength, flexibility, balance, endurance, and ability to be active, then after surgery you might have a harder time returning to your normal activities.footnote 1
Risks
Risks from knee replacement surgery include:
- Blood clots. People may get a blood clot in a leg vein after knee joint replacement surgery. Blood clots can be dangerous if they block blood flow from the leg back to the heart or move to the lungs. Blood clots occur more often in older people, people who are very overweight, people who have had blood clots before, and people who have cancer.
- Infection in the surgical wound or in the joint. Infection is rare in people who are otherwise healthy. Some people are at higher risk of infection after any surgery. This includes people who have other health problems, such as diabetes, rheumatoid arthritis, or chronic liver disease, and people who take corticosteroids. Most wound infections are treated with antibiotics. Infections deep in the joint may need more surgery. And in some cases the doctor must remove the artificial joint.
- Nerve injury. In rare cases, a nerve may be injured around the site of the surgery. It is more common (but still unusual) if the surgeon is also correcting problems in the joint. A nerve injury may cause tingling, numbness, or trouble moving a muscle. These injuries usually get better over time. In some cases they may go away completely.
- Problems with wound healing. Wound healing problems are more common in people who take corticosteroids or who have diseases that affect the immune system, such as rheumatoid arthritis and diabetes.
- Lack of good range of motion. How much you can bend your knee after surgery depends a lot on how much you could bend your knee before surgery. Some people are not able to bend their knee far enough to allow them to do their regular daily activities, even after several weeks of recovery. If this happens, the doctor may give you a medicine to relax your muscles and then gently force your knee to bend further. This may loosen tissues around the joint that are preventing you from bending it.
- Dislocation of the kneecap (patella). This is an uncommon complication of knee replacement surgery. If this happens, the kneecap may move to one side of the knee, and it will “pop” back when you bend your knee. This may not be painful, but it may make the knee feel unstable, and it may be uncomfortable. Dislocation of the kneecap interferes with the way your thigh muscles (quadriceps) work. It usually needs to be treated with surgery. In some cases, the knee replacement surgery must be completely redone if the dislocation is caused by a problem with the way the components in the knee line up.
- Fracture of the kneecap (patella). The kneecap could fracture either because of a fall or while you are using the knee normally. This complication is very uncommon. It may be seen in people who can bend the knee almost normally and can easily climb stairs and get up from chairs. Doctors usually can treat a fractured kneecap without surgery.
- Instability in the joint. The knee may be unstable or wobbly if the replacement components are not properly aligned. You may need a second surgery to align the components correctly so that your knee is stable.
- The usualrisks of general anesthesia. Risks of any surgery are higher in people who have had a recent heart attack and those who have long-term (chronic) lung, liver, kidney, or heart disease.
What To Think About
Exercise (swimming, walking) is important to your general well-being and muscle strength. Talk with your doctor about what type of exercise is best for you.
You may donate your own blood to use during surgery if needed. This is called autologous blood donation. If you choose to do this, start the donation several weeks before the surgery. You will have more time to donate enough blood and rebuild your blood volume before surgery.
If you need more than one joint replacement surgery, such as both knees or a knee and a hip, talk to your doctor about guidelines that may help you and your doctor decide in which order to do the surgeries.
References
Citations
- Sibanda N, et al. (2008). Revision rates after primary hip and knee replacement in England between 2003 and 2006. Public Library of Science Medicine, 5(9): 1398–1408.
Other Works Consulted
- American Academy of Orthopaedic Surgeons (2007). Activities after a knee replacement. Available online: http://orthoinfo.aaos.org/topic.cfm?topic=a00357.
- Rethman MP, et al. (2012). Prevention of Orthopaedic Implant Infection in Patients Undergoing Dental Procedures: Executive Summary on the AAOS/ADA Clinical Practice Guideline. Available online: http://www.aaos.org/research/guidelines/PUDP/dental_guideline.asp.
- Skou ST, et al. (2015). A randomized, controlled trial of total knee replacement. New England Journal of Medicine, 373(17): 1597–1606. DOI: 10.1056/NEJMoa1505467. Accessed December 11, 2015.
Credits
Current as of: June 26, 2019
Author: Healthwise Staff
Medical Review:Anne C. Poinier MD – Internal Medicine & E. Gregory Thompson MD – Internal Medicine & Adam Husney MD – Family Medicine & Kathleen Romito MD – Family Medicine & Kenneth J. Koval MD – Orthopedic Surgery, Orthopedic Trauma & David Bardana MD, FRCSC – Orthopedic Surgery, Sports Medicine
Current as of: June 26, 2019
Author: Healthwise Staff
Medical Review:Anne C. Poinier MD – Internal Medicine & E. Gregory Thompson MD – Internal Medicine & Adam Husney MD – Family Medicine & Kathleen Romito MD – Family Medicine & Kenneth J. Koval MD – Orthopedic Surgery, Orthopedic Trauma & David Bardana MD, FRCSC – Orthopedic Surgery, Sports Medicine
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.