Osteoarthritis
Topic Overview

What is osteoarthritis?
Osteoarthritis is a painful problem with the joints. Healthy joints help your body move, bend, and twist. Knees glide up and down stairs without creaking or crunching. Hips move you along on a walk without a complaint. But when you have arthritis, such simple, everyday movements can hurt. Using the stairs can be painful. Walking a few steps, opening a door, and even combing your hair can be hard.
Arthritis is mainly a disease of the spine, hip, hand, knee, and foot. But it can happen in other joints too. A joint is where two bones connect. And you have them all over your body.
Arthritis is most common in older people. Even though you can’t cure arthritis, there are many treatments that can help with your pain and make it easier for you to move. And you can do things to keep the damage from getting worse.
What causes osteoarthritis?
The simplest way to describe arthritis is that it’s wear and tear on the cartilage of your joints. This cushioning tissue is firm, thick, and slippery. It covers and protects the ends of bones where they meet to form a joint.
With arthritis, there are changes in the cartilage that cause it to break down. When it breaks down, the bones rub together and cause damage and pain. Experts don’t know why this breakdown in cartilage happens. But aging, joint injury, being overweight, and genetics may be a part of the reason.
What are the symptoms?
- Pain. Your joints may ache, or the pain may feel burning or sharp.
- Stiffness. Getting up in the morning can be hard. Your joints may feel stiff and creaky for a short time, until you get moving.
- Muscle weakness. The muscles around the joint may get weaker. This happens a lot with arthritis in the knee.
- Deformed joints. Joints can start to look like they are the wrong shape, especially as arthritis gets worse.
- Reduced range of motion and loss of use of the joint. As your arthritis gets worse, you may not be able to fully bend, flex, or extend your joints. Or you may not be able to use them at all.
- Cracking and creaking. Your joints may make crunching, creaking sounds.
How is osteoarthritis diagnosed?
Your doctor will check that your pain is not caused by another problem. He or she will ask questions about your symptoms, such as:
- Is the pain burning, aching, or sharp?
- Are your joints stiff in the morning? If yes, how long does the stiffness last?
- Do you have any joint swelling?
If your joints are tender and swollen and the muscles are weak, this will also help your doctor confirm whether you have arthritis. You may also have X-rays to check your joints for damage. Your doctor may want to do blood tests or other tests to see if there are other causes for your pain.
How is it treated?
There are many treatments for arthritis, but what works for someone else may not help you. Work with your doctor to find what is best for you. Often a mix of things helps the most.
Your treatment may include:
- Using pain medicine.If your pain is mild, over-the-counter pain medicines such as acetaminophen (for example, Tylenol) and nonsteroidal anti-inflammatory drugs (NSAIDs) may help. Commonly used NSAIDs include ibuprofen (such as Advil and Motrin) and naproxen (such as Aleve). But if these don’t get rid of your pain, you may need a stronger prescription medicine. Having shots of medicine in the joint also helps some people.
- Using heat or ice on the painful joint. Heat may help you loosen up before an activity. Ice is a good pain reliever after activity or exercise. Your doctor may give you gels or creams that you can rub on the joint to make it stop hurting.
- Losing weight, if you’re overweight. Losing weight may be one of the best things you can do for your arthritis. It helps take some of the stress off of your joints.
- Exercising to strengthen your muscles. Having stronger thigh muscles, for example, can help reduce stress on your knees. Swimming, biking, and walking are good activities. But make sure you talk to your doctor about what kind of activity is best for you. You may also get help from a physical therapist.
- Having surgery. If the pain in your hip or knee does not get better with treatment, you may decide to have surgery to replace the joint.
There are also some things you can do at home to help relieve your symptoms. For example, there are devices and tools that can take the stress and weight off of your joints and make it easier for you to hold objects, open and close things, and walk. Doorknob covers, tape, braces, splints, and canes may help.
You might also try changing activities or the way you do things to reduce the stress on the joint that hurts and allow you to move better. For example, walk instead of jog. Or use a sewing machine to make a quilt instead of making it by hand.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Cause
Osteoarthritis occurs when changes in cartilage cause it to break down and wear away. When cartilage breaks down, the bones rub together and cause damage and pain. Experts don’t know why this happens. But things like aging, joint injury, being overweight, and genetics may increase your risk.
In some cases, arthritis is caused by other conditions that damage cartilage.
Symptoms
Symptoms of osteoarthritis can range from mild to severe.
They may include:
- Pain. Your joints may ache, or the pain may feel burning or sharp. For some people, the pain may come and go. Constant pain or pain while you sleep may be a sign that your arthritis is getting worse.
- Stiffness. When you have arthritis, getting up in the morning can be hard. Your joints may feel stiff and creaky for a short time, until you get moving. You may also get stiff from sitting.
- Muscle weakness.The muscles around the joint may get weaker. This happens a lot with arthritis in the knee.
- Swelling. Osteoarthritis does not usually cause much swelling but may cause a little, especially in the knees.
- Deformed joints. Joints can start to look like they are the wrong shape, especially as arthritis gets worse.
- Reduced range of motion and loss of use of the joint. As your arthritis gets worse, you may not be able to fully bend, flex, or extend your joints. Or you may not be able to use them at all.
- Cracking and creaking. Your joints may make crunching, creaking sounds. This creaking may also occur in a normal joint. But in most cases, it doesn’t hurt and doesn’t mean that there is anything wrong with the joint.
- Sleep problems. The pain and stiffness of arthritis can disrupt sleep. And sleep problems may make it harder to cope with pain.
Arthritis of the spine can also narrow the openings that make space for the spinal cord and for the nerves that branch off the spinal cord (spinal nerves). This is called spinal stenosis. It can lead to pressure on the spinal cord or spinal nerves. This pressure can cause pain, weakness, or numbness.
Some medical conditions can cause symptoms similar to osteoarthritis, such as joint injuries and other forms of arthritis.
|
One Man’s Story:  Steve, 55 “I thought the stiffness and pain in my hip was just from the stress I was putting on my muscles. But when I changed my exercise routine or stopped working out, the pain was still there … The pain would come and go. It wasn’t a sharp pain, but a kind of ache that would keep me awake a lot. I could never stay in one position for very long.”— Steve Read more about Steve and how he learned to cope with arthritis. |
What Happens
Osteoarthritis occurs when the cartilage that cushions your joints breaks down and wears away. When this happens, the bones rub together and cause damage and pain. In most cases, it takes years for cartilage to break down.
It’s hard to know how fast arthritis may progress. You may not have any symptoms for years, until the bones and tissues become damaged. Or symptoms may come and go, stay the same, or get worse over time.
Arthritis can cause problems in any joint in the body. But in most cases, you’ll have symptoms in only one or two joints or groups of joints. Arthritis may cause problems in your hands, hips, knees, or feet, and sometimes in your spine. At first, you may only feel pain when you’re active. As the disease gets worse, you may also feel pain when you’re at rest.
If you have arthritis in your fingers, the joints at the tip or middle part of your fingers may get bigger and form bumps. These are known as Heberden’s and Bouchard’s nodes.
Even though there is no cure for arthritis, most people can manage their symptoms with medicine and lifestyle changes. But in a few people, arthritis or complications of arthritis may get so bad that they decide to have surgery to replace the worn joint or to fuse the bones together so that the joint won’t bend.
What Increases Your Risk
Things that can increase your risk for osteoarthritis are called risk factors. Some risk factors, such as your age or family history, can’t be changed or prevented.
You may be able to reduce other risk factors by making lifestyle changes or taking medicine.
Risk factors you may be able to change or prevent
- Being overweight. Extra weight puts added stress on your joints and can change the normal shape of the joint.
- Joint injury. A single major injury to a joint or several minor injuries can cause cartilage damage over time. Activities that put repeated stress on a joint include squatting, kneeling, or heavy lifting common to some sports and jobs.
- Lack of exercise, which can cause your muscles and joints to get weak and stiff.
Risk factors you can’t change
- Getting older. Age is not a direct cause of arthritis, but as you get older you’re more likely to have symptoms. Still, not all older adults will have joint pain.
- Afamily history of arthritis.
- Loose or odd-shaped joints. Knees that bend outward (bowleg) or knees that bend toward each other (knock knees), for example, can cause an imbalance in the joints, because the cartilage wears down at an uneven rate.
- A previous infection of the joint.
- Other types of arthritis, such as rheumatoid arthritis or psoriatic arthritis.
- Metabolic or endocrine problems. These include a buildup of iron (hemochromatosis), copper (Wilson’s disease), or calcium (hyperparathyroidism) in the blood and tissues of the body.
- Decreased nerve function.
When should you call your doctor?
Call your doctor if you have:
- Sudden, unexplained swelling, warmth, or pain in any joint.
- Joint pain with a fever or rash.
- Pain so bad that you can’t use your joint.
- Mild joint symptoms that last more than 6 weeks and don’t get better with home treatment.
- Side effects from pain medicine. You can have side effects when you take large doses of pain medicine. Do not take more than the recommended dose of medicine without first talking to your doctor.
Watchful waiting
If you have mild joint pain and stiffness, first try home treatment, such as using ice and heat. If you don’t feel better in 6 weeks, or if you have other symptoms, call your doctor.
Who to see
Arthritis can be managed by:
- A family medicine physician.
- An internist.
- A nurse practitioner.
- A physician assistant.
- A rheumatologist.
Other health professionals may be part of the treatment team, such as:
Exams and Tests
In most cases, your doctor can tell you if you have osteoarthritis and recommend treatment based on your symptoms and by doing a physical exam. Your doctor may also do some other tests to be sure that the diagnosis is correct or to rule out other conditions that have similar symptoms.
These tests may include:
- A joint fluid study. A sample of the fluid that cushions the joint is removed and sent to the lab to look for the cause of joint pain and swelling.
- X-rays. Pictures of the bones in a joint, such as the hip or knee, are taken to look for cartilage damage.
Other tests may include a urine test and one or more blood tests, such as:
Treatment Overview
Even though there is no cure for osteoarthritis, treatment can help reduce your symptoms and make it possible for you to lead a full and active life.
The goals of treatment are to:
- Reduce your pain and stiffness.
- Keep your joints working and moving well.
- Keep you from becoming disabled.
- Prevent more damage to your joints.
Treatment is based on:
- How bad your symptoms are.
- How much your symptoms prevent you from doing your daily tasks.
- How well other treatments have worked.
- How much damage to the joint (or joints) you have.
Treatment for mild to moderate arthritis
In most cases, people who have mild to moderate arthritis can manage their symptoms for many years with a treatment plan that may include:
- Medicines, including acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen. Or you may use capsaicin cream on your skin.
- Exercise to help keep your muscles strong and your joints moving well.
- Weight loss, if you’re overweight, to reduce the stress on your joints.
- Heat and cold therapy, such as hot compresses, cold packs, ice massage, or paraffin wax.
- Physical therapyor occupational therapy.
- Assistive devices and orthotics, such as tape, braces, splints, or canes to help protect your joints from injury and take the stress off of your joints.
- Changing activities or the way you do things to rest or reduce the stress on the painful joint and allow you to move better.
- Learning and practicing a “good-health attitude” to help you cope with the stress and challenges of living with arthritis.
Some people with arthritis also feel down or depressed. They may describe this as feeling “depressed,” “unhappy,” “short-tempered,” “blue,” or “down in the dumps.” If you feel like this most of the time, tell your doctor. Treating these symptoms may help you feel better and make it easier for you to do your daily tasks.
Treatment if arthritis gets worse
If the pain and stiffness from arthritis don’t get better or they get worse, your doctor may recommend:
- Steroid shots.
- Pain medicine called tramadol.
- Opioid pain medicines.
- Physical therapy or occupational therapy.
If your pain is very bad, you may decide to have surgery to replace the joint. Or you may decide to have some other kind of surgery that can help keep your joints moving well and prevent your arthritis from getting worse.
Some types of surgery include:
- Arthrodesis.
- Arthroscopy.
- Finger or toe surgery.
- Joint replacement (hip, knee, or shoulder).
- Osteotomy (knee or hip).
For help deciding whether to have joint replacement surgery, see:
Prevention
You can take steps to help prevent osteoarthritis. If you already have arthritis, these same steps may keep it from getting worse.
- Stay at a healthy weight or lose weight if you need to. Extra weight puts a lot of stress on the large, weight-bearing joints such as the knees, the hips, and the balls of the feet. Experts estimate that every 1 lb (0.5 kg) of body weight adds about 4 lb (1.8 kg) of stress to the knee.footnote 1 This means that if you lost just 5 lb (2.3 kg), you could take 20 lb (9.1 kg) of stress off your knees.
- Be active. A lack of exercise can cause your muscles and joints to become weak. But light to moderate exercise can help keep your muscles strong and reduce joint pain and stiffness. For example, if your quadriceps (the muscles in the front of your thigh) are weak, you may be more likely to get arthritis of the knee.
- Protect your joints. Try not to do tasks that cause pain or swelling in joints. And try to use the largest joints or strongest muscles to do things. A single major injury to a joint or several minor injuries can damage cartilage over time.
Home Treatment
When you have osteoarthritis, you may find it hard to do your daily tasks. Your joints may ache or feel stiff, and they may hurt when you move. You can do some things at home to feel better.
Lifestyle changes
- Rest. If your joints hurt a lot or are swollen, take a break. But try not to let too much time pass before you get moving again. A lack of activity can cause your muscles and joints to become weak. Getting enough sleep can help your mood and help you cope with pain. If you are having trouble sleeping, talk to your doctor.
- Stay at a healthy weight. Being overweight puts extra stress on your joints. But losing weight can help. It can decrease the symptoms of osteoarthritis and allow you to be more active.footnote 2
- Exercise. Some people may be reluctant to exercise when they have arthritis, but it can help reduce pain and improve balance. Try exercises that don’t put a lot of stress on your joints, such as swimming, biking, walking, water exercises, and lifting light weights. And consider taking an exercise class designed for people who have arthritis. Many fitness clubs, community centers, and senior centers offer these classes. Be sure to talk to your doctor or physical therapist about what kind of activity is best for you.
Use devices
- Use assistive devices and orthotics. There are devices and tools that can take the stress and weight off your joints and make it easier for you to hold objects, open and close things, and walk. For example, doorknob covers, tape, braces, splints, and canes may help.
Change how you do things
- Protect your joints. There are some things that you can do to protect your joints. For example:
- Try not to do tasks that cause pain or swelling in joints.
- Use the largest joints or strongest muscles to do things. For example, when you lift a heavy object off the floor, use your hip and knee muscles, not your back. Or when you carry a bag of groceries, use the palm of your hand or your forearm instead of grasping it with your fingers.
- Change activities. If your joints hurt when you do an activity, try other ways of doing it that don’t cause pain. For example, walk instead of jog. Or use a sewing machine to make a quilt instead of making it by hand.
- Modify your home and work area. If you have a hard time moving around or if you get tired easily, try making some changes in your home and work areas. For example, use a reacher to pick up things off the floor. Or for tasks that you would normally do standing up, use a tall stool instead so you can sit down.
- Maintain good posture. Poor posture puts stress on your back and neck. The key to good posture is to keep the right amount of curve in your lower back. Too much curve (swayback) or too little (flat back) can cause problems. Having good posture can help reduce pain.
- Wear comfortable and supportive shoes. If you have arthritis in your back, hips, knees, or feet, you may be able to reduce the stress on your joints by wearing the right shoes or by adding insoles to your shoes. Talk to your doctor or physical therapist about the footwear that would be best for you.
Use medicine and heat or cold
- Use over-the-counter pain medicines, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen. Be safe with medicines. Read and follow all instructions on the label.
- Use heat and cold therapy, such as hot compresses, cold packs, or ice massage.
|
One Woman’s Story:  Bev, 76 “Gardening books and magazines always have wonderful ideas and innovations that you can use. For instance, I’ve cut off sections of the rubber insulation that is used to cover water pipes and slipped them over any of the garden tools that I’m going to use, because it gives me a little more cushion and a little extra width for my tools.”— Bev Read more about Bev and how she learned to cope with arthritis. |
Coping and support
Living with arthritis can be stressful. At times you may feel overwhelmed, tired, and angry. And you may worry about what your life may be like as your condition gets worse. These feelings are normal. But there are a lot of ways to cope with arthritis. For example, ask for help when you need it, keep a positive attitude, and join a support group.
If you are caring for someone who has arthritis, be sure to take time to care for yourself and find ways to manage stress. Being a caregiver isn’t easy. But it can be rewarding, especially when you know that your care makes a positive difference in someone’s life.
Medications
Medicine can help reduce your symptoms of osteoarthritis and allow you to do your daily activities.
The goal of medicine is to:
- Get rid of pain and have few side effects.
- Keep your joints working and moving well. If pain keeps you from moving your joints, it can cause the ligaments, tendons, and muscles that move your joints to shorten and become tight and weak.
The type of medicine depends on how bad your pain is. For instance:
- For mild to moderate pain, you can try over-the-counter pain medicine, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen.
- For moderate to severe pain, you may need stronger pain medicine such as opioids.
Medicine choices
Medicines used to treat arthritis include:
- Acetaminophen to help relieve pain.
- Nonsteroidal anti-inflammatory drugs to reduce pain, swelling, and fever.
- Tramadol to help relieve pain.
- Steroid shots in the joint to reduce swelling.
- Some antidepressants, such as duloxetine, to help relieve pain.
- Opioids to relieve moderate to severe pain.
Medicine that you put on your skin (topical) may relieve pain for a short time.footnote 3 These include topical NSAIDs, capsaicin, and pain-relieving creams.
What to think about
Before you take medicine
Here are a few things to think about:
- Medicine doesn’t cure arthritis or slow the time it takes for cartilage to break down. But it can help reduce pain and stiffness, which can make it easier for you to move.
- Medicine should be used along with other treatments, such as exercise and physical therapy, to help keep your joints working and moving well.
- If you have certain health problems, you may not be able to take some kinds of pain medicine. Be sure to tell your doctor if you have a history of bleeding in your stomach or another part of your digestive tract. And tell your doctor if you have a stomach ulcer, kidney problems, or heart failure, or if you take a blood-thinner medicine.
Effects of medicines
Medicines that work for some people don’t work for others. Be sure to let your doctor know if the medicine you’re taking doesn’t help. You may need to try several kinds of medicines to find one that works for you.
Be safe with medicines. Read and follow all instructions on the label.
Here are a few things to think about:
- The medicine you take may cause side effects. Your doctor may suggest that you first try acetaminophen, because it has fewer side effects than any other pain medicine used for arthritis.
- Most studies suggest that nonsteroidal anti-inflammatory drugs (NSAIDs) work better than acetaminophen for arthritis. But for some people, acetaminophen may work as well as NSAIDs for mild to moderate joint pain. And studies show that acetaminophen is better than no treatment.footnote 4
- If you can’t take NSAIDs, and if other treatments haven’t worked, your doctor may prescribe opioids. When taken as prescribed, they can be a safe and effective way to relieve pain.
- Because you’ll likely take medicine for a long time, you’ll need to see your doctor for regular checkups to look for any side effects that may develop from long-term use. He or she may prescribe medicine that can help prevent stomach ulcers, which may develop when you take pain medicine every day.
Surgery
In most cases, people can manage their osteoarthritis symptoms with medicine and lifestyle changes. But surgery may be an option if:
- You have very bad pain.
- You have lost a lot of cartilage.
- You have tried medicine and other treatments, but they haven’t helped.
- Your overall health is good.
|
One Man’s Story:  Steve, 55 “I wasn’t sure about having surgery since I was so young. I had heard that an artificial hip could give out in 10 to 20 years … But when the medicine I was taking stopped working, I figured I had gone as far as I could go with this, and decided to go ahead with the surgery … It’s a strange feeling to be able to walk without a limp and to walk up and down stairs without grabbing on to the railing.”— Steve Read more about Steve and how he learned to cope with arthritis. |
Surgery choices
Types of surgery for arthritis include:
- Arthrodesis. This joins (fuses) two bones in a damaged joint so that the joint won’t bend. Doctors may use it to treat arthritis of the spine, ankles, hands, and feet. In rare cases, it’s used to treat the knees and hips.
- Arthroscopy. This may be used to smooth a rough joint surface or remove loose cartilage or bone fragments. In some people it may help relieve pain for a short time and allow the joint to move better.
- Hip resurfacing surgery. This is most often done in younger, more active people who have pain and disability caused by a badly damaged hip.
- Joint replacement. This is done when other treatments haven’t worked and damage to the joint can be seen on X-rays. It involves surgery to replace the ends of bones in a damaged joint. The surgery creates new joint surfaces. The joints that are replaced most often are the hip, knee, and shoulder. But other joints such as the elbow and the ankle can also be replaced.
- Osteotomy. This is done to correct certain defects in the hip and knee. In most cases, it’s done in active people younger than 60 who want to delay surgery to replace a hip or knee.
Small joint surgery. Surgery is more common on the larger joints, such as the hip and the knee. But if pain in the small joints of the hands or feet is so bad that the person can’t use those joints, surgery may help.
A newer procedure for arthritis of the knee uses a small cup shaped like a “C.” It’s placed in the joint space of the inner knee and acts as a cushion for the joint. It may help delay surgery to replace the knee.
What to think about
Before deciding to have surgery
If you’re in poor health or have certain health problems, you may not be able to have surgery. Your doctor can help you decide if surgery is right for you.
Here are some things to think about if you’re thinking about surgery:
- After surgery, most people are able to go back to doing their daily tasks and sports with less pain.
- You will need several months of physical therapy to get the best use of your joint.
- Replacement joints typically last 10 to 20 years. You may need another surgery if the new joint wears out.
- If you have already lost a lot of your strength, flexibility, balance, endurance, and ability to be active before you have surgery, then after the surgery you might have a harder time returning to your normal activities.
For help deciding whether to have joint replacement surgery, see:
If you decide to have surgery
In the days or weeks before your surgery, talk to your doctor about what you need to do to get ready for your return home. For example, you may need to arrange for someone to drive you home and to help you after your surgery. Or you may need to make changes to your home, such as removing small rugs, to help you move around.
Other Treatment
Many people use some form of complementary medicine to treat certain health problems, including osteoarthritis. These treatments are often used along with standard care to help relieve their arthritis symptoms.
Some of these treatments may help you move more easily and deal with the stress and pain of arthritis. But in some cases, not much is known about how safe they are or how well they may work.
Be sure to tell your doctor if you’re using a complementary therapy or if you’re thinking about trying one. He or she can discuss the possible benefits and potential side effects of these treatments and whether any of these treatments may interfere with your standard care. For example, some diet supplements and herbal medicines may cause problems if you take them with another medicine.
Complementary medicine
- Dietary supplements to try to relieve pain and stiffness. Examples include:
- Avocado/soybean (ASU) extract.
- Boron.
- Fish oil.
- Glucosamine and chondroitin.
- S-adenosylmethionine (SAM-e).
- Vitamins B3, C, and E.
- Acupuncture. Acupuncture involves putting very tiny needles into your skin at certain places on your body to try to relieve pain.
- Mind and body practices, such as yoga, tai chi, and qi gong, can help reduce stress and relax your mind and muscles.
Other treatments to consider
- Taping uses tape that sticks to the knee to help keep the kneecap in place and relieve pain. You can do taping at home. But first have your doctor or physical therapist show you the right way to put it on.
- Braces can help shift weight off the part of your knee that hurts. It’s not clear how well these work, but there isn’t a lot of risk in trying them.
- Capsaicin is a cream that you put on your skin for pain relief.
- Pulsed electromagnetic field therapy uses magnets to produce an electrical pulse that may help cartilage grow.
- Transcutaneous electrical nerve stimulation, or TENS, uses a mild electrical current to reduce pain.
|
One Woman’s Story:  Bev, 76 “After I have a massage and acupuncture, I feel like a new person. I encourage people to find out what treatments others have tried and what things have worked for them. I’m a believer in other people’s ideas. Obviously, what works for one person may not work for another, but unless you try it, you’ll never know if it’ll help.”— Bev Read more about Bev and how she learned to cope with arthritis. |
What to think about
There are many treatments for arthritis, but what works for someone else may not work for you. You may need to try several different treatments to find what works for you.
Experts are testing new medicines and methods that they hope will one day help prevent, reduce, or repair cartilage damage. For example, they’re looking at cartilage transplants and the use of stem cells to grow new cartilage. So far, therapies to repair cartilage have only been studied in younger people with small, well-defined holes in their knee cartilage. This isn’t a common problem for most older adults who have arthritis of the knee.
References
Citations
- Messier SP, et al. (2005). Weight loss reduces knee-joint loads in overweight and obese older adults with knee osteoarthritis. Arthritis and Rheumatism, 52(7): 2026–2032.
- Stitik TP, et al. (2010). Osteoarthritis. In WR Frontera et al., eds., DeLisa’s Physical Medicine and Rehabilitation: Principles and Practice, 5th ed., vol. 1, pp. 781–809. Philadelphia: Lippincott Williams and Wilkins.
- Lozada CJ (2013). Treatment of osteoarthritis. In GS Firestein et al., eds., Kelley’s Textbook of Rheumatology 9th ed., vol. 2, pp. 1646–1659. Philadelphia: Saunders.
- Towheed TE, et al. (2006). Acetaminophen for osteoarthritis. Cochrane Database of Systematic Reviews (1). Oxford: Update Software.
Other Works Consulted
- American Academy of Orthopaedic Surgeons (2013). Summary of recommendations. Treatment of Osteoarthritis of the Knee, 2nd ed. Available online: http://www.aaos.org/research/guidelines/guidelineoaknee.asp.
- Derry S, et al. (2012). Topical NSAIDs for chronic musculoskeletal pain in adults. Cochrane Database of Systematic Reviews (9).
- Dunlop DD, et al. (2011). Physical activity levels and functional performance in the Osteoarthritis Initiative. Arthritis and Rheumatism, 63(1): 127–136.
- Easley ME, et al. (2011). Results of total ankle arthroplasty. Journal of Bone and Joint Surgery, American Version, 93(15): 1455–1468.
- Hinman RS, et al. (2014). Acupuncture for chronic knee pain: A randomized clinical trial. JAMA, 312(13): 1313–13222. DOI: 10.1001/jama.2014.12660. Accessed July 23, 2015.
- Hochberg MC, et al. (2012). American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care & Research, 64(4): 465–474.
- Li S, Micheletti R (2011). Role of diet in rheumatic disease. Rheumatic Disease Clinics of North America, 37(1): 119–133.
- Lin EHB, et al. (2003). Effect of improving depression care on pain and functional outcomes among older adults with arthritis: A randomized controlled trial. JAMA, 290(18): 2428–2434.
- Louie GH, et al. (2011). Sleep disturbances in adults with arthritis: Prevalence, mediators, and subgroups at greatest risk. Data from the 2007 national health interview survey. Arthritis Care and Research, 63(2): 247–260.
- Peak EL, et al. (2005). The role of patient restrictions in reducing the prevalence of early dislocation following total hip arthroplasty. Journal of Bone and Joint Surgery, 87-A(2): 847–853.
Credits
Current as ofApril 1, 2019
Author: Healthwise Staff
Medical Review: Anne C. Poinier, MD – Internal Medicine
Adam Husney, MD – Family Medicine
E. Gregory Thompson, MD – Internal Medicine
Martin J. Gabica, MD – Family Medicine
Kathleen Romito, MD – Family Medicine
Stanford M. Shoor, MD – Rheumatology
Current as of: April 1, 2019
Author: Healthwise Staff
Medical Review:Anne C. Poinier, MD – Internal Medicine & Adam Husney, MD – Family Medicine & E. Gregory Thompson, MD – Internal Medicine & Martin J. Gabica, MD – Family Medicine & Kathleen Romito, MD – Family Medicine & Stanford M. Shoor, MD – Rheumatology
 Joints Often Affected by Osteoarthritis
Joints Often Affected by Osteoarthritis Cartilage of the Knee
Cartilage of the Knee Osteoarthritis of the Hand
Osteoarthritis of the Hand Osteoarthritis of the Hip
Osteoarthritis of the Hip Osteoarthritis of the Knee
Osteoarthritis of the Knee Osteoarthritis of the Foot
Osteoarthritis of the Foot Osteoarthritis of the Spine
Osteoarthritis of the Spine Heberden’s and Bouchard’s Nodes
Heberden’s and Bouchard’s Nodes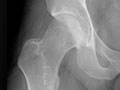 X-Ray of Osteoarthritis of the Hip
X-Ray of Osteoarthritis of the Hip X-Ray of Osteoarthritis of the Knee
X-Ray of Osteoarthritis of the Knee Hot and Cold Therapy for Arthritis
Hot and Cold Therapy for Arthritis Arthritis: Making Everyday Activities Easier
Arthritis: Making Everyday Activities Easier Exercising Safely With Arthritis
Exercising Safely With Arthritis Knee Arthritis: What Is Osteoarthritis?
Knee Arthritis: What Is Osteoarthritis? Knee Arthritis: What Can I Expect?
Knee Arthritis: What Can I Expect?
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.

