Colorectal Cancer
Topic Overview
Is this topic for you?
This topic will tell you about the early testing, diagnosis, and treatment of colorectal cancer. If you want to learn about colorectal cancer that has come back or has spread, see the topic Colorectal Cancer, Metastatic or Recurrent.If you want to learn about anal cancer, see the topic Anal Cancer.
What is colorectal cancer?
Colorectal cancer means that cells that aren’t normal are growing in your colon or rectum. These cells grow together and form polyps. Over time, some polyps can turn into cancer.
This cancer is also called colon cancer or rectal cancer, depending on where the cancer is. It is the third most common cancer in the United States. And it occurs most often in people older than 50.
What causes colorectal cancer?
The exact cause of colorectal cancer is not known. Most cases begin as small growths, or polyps, inside the colon or rectum.
Colon polyps are very common. If they are found early, usually through routine screening tests, they can be removed before they turn into cancer.
What are the symptoms?
Colorectal cancer usually doesn’t cause symptoms until after it has started to spread. See your doctor if you have any of these symptoms:
- Pain in your belly
- Blood in your stool or very dark stools
- A change in your bowel habits, such as more frequent stools or a feeling that your bowels are not emptying completely
How is colorectal cancer diagnosed?
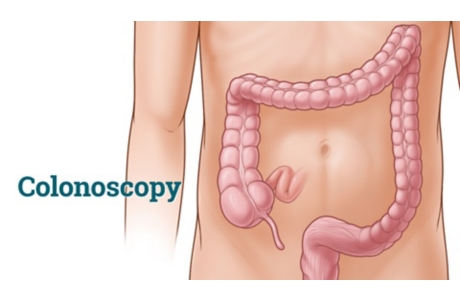
If your doctor thinks that you may have this cancer, you will need a test, called a colonoscopy (say “koh-luh-NAW-skuh-pee”), that lets the doctor see the inside of your entire colon and rectum. During this test, your doctor will remove polyps or take tissue samples from any areas that don’t look normal. The tissue will be looked at under a microscope to see if it contains cancer.
Sometimes another test, such as a sigmoidoscopy (say “sig-moy-DAW-skuh-pee”), is used to diagnose colorectal cancer.
How is it treated?
Colorectal cancer is usually treated with surgery, chemotherapy, radiation, or targeted therapy. Rectal cancer may be treated with immunotherapy.
How can you screen for colorectal cancer?
Screening tests can find or prevent many cases of colon and rectal cancer. They look for a certain disease or condition before any symptoms appear. Some experts say that adults should start regular screening at age 50 and stop at age 75. Others say to start before age 50 or continue after age 75. Talk with your doctor about your risk and when to start and stop screening. Your doctor may recommend getting tested more often or at a younger age if you have a higher risk.
Screening tests include stool tests, such as FIT, that can be done at home and procedures, such as colonoscopy, that are done at your doctor’s office or clinic.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Cause
Most cases begin as polyps, which are small growths inside the colon or rectum. Colon polyps are very common. Some polyps can turn into cancer.
Some people have a medical or family history that can increase their risk for colorectal cancer. Because of their history, they may be more likely to develop polyps that could turn into colorectal cancer.
Symptoms
Colorectal cancer in its early stages usually doesn’t cause any symptoms. Symptoms occur later, when the cancer may be harder to treat. The most common symptoms include:
- Pain in the belly.
- Blood in your stool or very dark stools.
- A change in your bowel habits. (You may have more frequent stools or a feeling that your bowels aren’t emptying completely).
- Constant tiredness (fatigue).
- In rare cases, unexplained weight loss.
What Happens
How cancer grows and spreads
Cancer is the growth of abnormal cells in the body. These extra cells grow together and form masses, called tumors. In colorectal cancer, these growths usually start as polyps in the large intestine (colon or rectum). If colon polyps aren’t found and removed, they may turn into cancer.
Cancers in the colon or rectum usually grow very slowly. It takes most of them years to become large enough to cause symptoms. If the cancer is allowed to grow, over time it will invade and destroy nearby tissues and then spread farther. Colorectal cancer spreads first to nearby lymph nodes. From there it may spread to other parts of the body, usually the liver. It may also spread to the lungs, and less often, to other organs in the body.
Survival rates
The long-term outcome, or prognosis, for colorectal cancer depends on how much the cancer has grown and spread. Experts talk about prognosis in terms of “5-year survival rates.” This means the percentage of people who are still alive 5 years or longer after their cancer was found. It is important to remember that these are only averages. Everyone’s case is different. And these numbers don’t necessarily show what will happen to you. The estimated 5-year survival rate for colorectal cancer is:footnote 1
- 90% or more if cancer is found early and treated before it has spread. This means that 90 or more out of 100 people will still be alive in 5 years if the cancer is found early and treated before it has spread.
- 71% if the cancer has spread to nearby organs and lymph nodes. This means that 71 out of 100 people will still be alive in 5 years if the cancer has spread to nearby organs and lymph nodes.
- 14% if the cancer has spread to the liver, lungs, or bones. This means that 14 out of 100 people will still be alive in 5 years if the cancer has spread to the liver, lungs, or other organs in the body.
These numbers are taken from reports that were done from 2007 to 2013, before newer treatments were available. So the actual chances of your survival are likely to be higher than these numbers.
What Increases Your Risk
A risk factor for colorectal cancer is something that increases your chance of getting this cancer. Having one or more of these risk factors can make it more likely that you will get colorectal cancer. But it doesn’t mean that you will definitely get it. And many people who get colorectal cancer don’t have any of these risk factors.
Risks you can change
There are lifestyle actions you can take to lower some of the risk factors for colorectal cancer. These actions include:
- Maintain a healthy weight.
- Be physically active.
- Eat healthy foods, including vegetables, fruits, and whole grains. Avoid eating a lot of red meat or processed meats.
- If you smoke, get help to quit.
- If you drink alcohol, limit how much you drink.
Risks you can’t change
Your age
Getting older is a risk factor for colorectal cancer.
Your race and ethnicity
African Americans have a higher risk of getting colorectal cancer (and dying from it) than people of other races. And Ashkenazi Jews (Jewish people whose ancestors came from Eastern Europe) who have inherited certain genes are also at a higher risk for getting colorectal cancer.
Your family’s medical history
You are more likely to get colorectal cancer if one of your parents, brothers, sisters, or children has had the disease. Your risk is higher if this family member had colorectal cancer younger than 45 years old, or if more than one family member had the disease.
Some common gene changes increase the chance of colorectal cancer. These changes are familial adenomatous polyposis (FAP) and Lynch syndrome, also called hereditary nonpolyposis colorectal cancer (HNPCC). Many people with these changed genes will get colorectal cancer if they aren’t carefully watched. Genetic testing can tell you if you carry a changed, or mutated, gene that can cause FAP or HNPCC.
Your medical history
Your chances of getting colorectal cancer are higher if you have had:
- Colorectal cancer in the past.
- Another type of cancer, such as cancer of the ovary or cancer of the endometrium.
- Adenomatous polyps removed from your colon.
- Ulcerative colitis or Crohn’s disease.
- Radiation therapy in your abdomen or pelvis.
When should you call your doctor?
Call your doctor if you have any symptoms of colorectal cancer, such as:
- A change in bowel habits.
- Bleeding from your rectum, including bright red or dark blood in your stools or stools that look black.
- Constant or frequent diarrhea, constipation, or a feeling that your bowel doesn’t empty completely.
- Stools that are narrow (may be as narrow as a pencil).
- Belly pain or problems with gas or bloating.
- Unexplained weight loss.
- Constant tiredness (fatigue).
Because colorectal cancer often doesn’t cause any symptoms, talk with your doctor about screening tests. Screening helps doctors find a certain disease or condition before any symptoms appear.
Who to see
Health professionals who can evaluate your symptoms of colorectal cancer include:
- Family medicine doctors.
- General practitioners.
- Gastroenterologists.
- General surgeons and colorectal surgeons.
- Internists.
- Nurse practitioners.
- Physician assistants.
If your doctor thinks you may have colorectal cancer, he or she may advise you to see a general surgeon or a colorectal surgeon. Colorectal cancer is treated by surgeons, medical oncologists, and radiation oncologists.
Exams and Tests
If your doctor thinks you may have colorectal cancer, he or she will ask you questions about your medical history and give you a physical exam. Other tests may include:
- A colonoscopy. Your doctor uses a lighted scope to view the inside of your entire colon. Polyps can be removed during this test. A colonoscopy is recommended when another screening test shows that you may have colorectal cancer.footnote 2
- A sigmoidoscopy. Your doctor uses a lighted scope to view the lower part of your intestine. Doctors can also remove polyps during this test.
- A barium enema. A whitish liquid with barium is inserted through your rectum into your intestine. The barium outlines the inside of the colon so that it can be seen on an X-ray.
- A biopsy. A sample of tissue is taken from the inside of your intestine and examined under a microscope. A doctor called a pathologist can look at the tissue sample and see if it contains cancer.
- A complete blood count, which is a blood test. It is used to look into symptoms such as fatigue, weakness, anemia, bruising, or weight loss.
For people who have an increased risk for colorectal cancer, regular colonoscopy is the recommended screening test. It allows your doctor to remove polyps (polypectomy) and take tissue samples at the same time.
When you are diagnosed with colorectal cancer, your doctor may order other tests to find out if the cancer has spread. These tests include:
- A CT scan to see if the cancer has spread to your liver, lungs, or belly.
- A chest X-ray to see if the cancer has spread to your lungs.
- An MRI or PET scan to see if the cancer has spread into your chest or organs in the belly or pelvis.
- An ultrasound to find the cause of belly pain or increased belly girth. It can also see if the cancer has spread to your liver. An endoscopic ultrasound is used to see how far rectal cancer may have spread.
- A blood chemistry panel to see if the cancer has spread to your liver and bones.
- A carcinoembryonic antigen (CEA) blood test to check the level of this tumor marker.
Early detection
Routine screening can reduce deaths from colorectal cancer.
Your risk for colorectal cancer gets higher as you get older. Some experts say that adults should start regular screening at age 50 and stop at age 75. Others say to start before age 50 or continue after age 75. Talk with your doctor about your risk and when to start and stop screening.
Treatment Overview
You and your doctor will work together to decide what your treatment should be. You will consider your own preferences and your general health. But the stage of your cancer is the most important tool for choosing your treatment. Staging is a way for your doctor to tell how far, if at all, your cancer has spread.
Surgery
Surgery is almost always used to remove colorectal cancer. Sometimes a simple operation can be done during a colonoscopy or sigmoidoscopy to remove small polyps and a small amount of tissue around them. But in most cases, a major operation is needed to remove the cancer and part of the colon or rectum around it. If cancer has spread to another part of your body, such as the liver, you may need more far-reaching surgery.
Chemotherapy
Chemotherapy uses medicines to destroy cancer cells throughout the body. Several medicines are often used together.
Radiation therapy
Radiation therapy uses X-rays to destroy cancer cells. This is used for some types of cancer in the rectum. Radiation therapy is often combined with surgery or chemotherapy. To learn more, see Other Treatment.
Cancers that have not spread beyond the colon or rectum may need only surgery. If the cancer has spread, you may need radiation therapy, chemotherapy, or both.
Targeted therapy
This treatment uses medicines called monoclonal antibodies to treat colorectal cancer. It is often given along with chemotherapy.
Immunotherapy
Rectal cancer may be treated with immunotherapy. This treatment uses the body’s own immune system against cancer cells. It may be used as a treatment for rectal cancer.
Side effects of treatment
Surgery, chemotherapy, and radiation can have serious side effects. But your medical team will help you manage the side effects of your treatment. This may include medicines for pain after surgery or medicines to control nausea and vomiting if you have chemotherapy.
Talk with your doctor and medical team about your side effects. Some side effects, such as pain or tingling in your hands or feet that gets worse (peripheral neuropathy), may be a sign that your medicines need to be changed.
For tips on how to manage side effects at home, see Home Treatment.
Regular checkups
After you have had colorectal cancer, your chances of having it again go up. It’s important to keep seeing your doctor and be tested regularly to help find any returning cancer or new polyps early. After your treatment, you will need regular checkups by a family doctor, general practitioner, medical oncologist, radiation oncologist, or surgeon, depending on your case.
When cancer comes back or spreads
Colorectal cancer comes back in about half of people who have surgery to remove the cancer.footnote 3 The cancer may be more likely to come back after surgery if it was not found in an early stage. Cancer that has spread or comes back is harder to treat, but sometimes treatments are successful. For more information, see the topic Colorectal Cancer, Metastatic and Recurrent.
Support and resources
Finding out that you have cancer can change your life. You may feel like your world has turned upside down and you have lost all control. Talking with family, friends, or a counselor can really help. Ask your doctor about support groups. Or call the American Cancer Society (1-800-227-2345) or visit its website at www.cancer.org.
To learn more about colon and rectal cancer, go to the website of the National Cancer Institute at www.cancer.gov/cancertopics/types/colon-and-rectal.
Prevention
Screening for colorectal cancer
Screening tests look for a certain disease or condition before any symptoms appear. Your risk for colorectal cancer gets higher as you get older. Some experts say that adults should start regular screening at age 50 and stop at age 75. Others say to start before age 50 or continue after age 75. Talk with your doctor about your risk and when to start and stop screening.
Your doctor may recommend earlier and more frequent testing if you have a higher risk for colorectal cancer.
For more information, see:
Genetic testing
If you have a very strong family history of colorectal cancer, you may want to talk to your doctor or a genetic counselor about having a blood test to look for changed genes. Genetic testing can tell you if you carry a changed, or mutated, gene that can cause colorectal cancer. Having certain genes greatly increases your risk of colorectal cancer. But most cases of colorectal cancer aren’t caused by changed genes.
Home Treatment
Managing side effects
During treatment for colorectal cancer, you can do things at home to help manage your side effects and symptoms. If your doctor has given you instructions or medicines to treat these problems, be sure to also use them.
In general, healthy habits such as eating a balanced diet and getting enough sleep and exercise may help control your symptoms.
You can try home treatments:
- For nausea or vomiting, such as ginger tea, peppermint candy or gum, or drinking enough fluids so that you don’t get dehydrated.
- For diarrhea, such as taking small, frequent sips of water and bites of salty crackers.
- For constipation, such as getting plenty of water and fiber in your diet. Do not use a laxative without first talking to your doctor.
Other problems that can be treated at home include:
- Sleep problems. If you have trouble sleeping, try having a regular bedtime, getting exercise daily, and avoiding caffeine late in the day.
- Feeling very tired. If you lack energy or become weak easily, try to get extra rest and plan your schedule to make the most of the energy you have.
- Pain. There are many home treatments that can help when you have pain, such as over-the-counter pain relievers, heat packs, or cold packs. Talk to your doctor before using any home treatment for pain.
- Mouth sores. This includes watching what you eat and drink and rinsing regularly with mouthwash or an antacid.
Managing stress from having cancer
Having cancer can be very stressful. Finding new ways of coping with your stress may improve your overall quality of life.
These ideas may help:
- Take steps to reduce your stress. Find new ways to relax, such as yoga or visualization exercises.
- Get the support you need. Spend time with people who care about you. Let them help you.
- Talk about your feelings. Try meeting with a counselor or joining a support group where you can share your experience.
- Ask your doctor to help you find other sources of support and information.
Your feelings about your body may change after treatment. Dealing with your body image may involve talking openly with your partner about your worries and discussing your feelings with a doctor.
Having cancer can change your life in many ways. For help with managing these changes, see the topic Getting Support When You Have Cancer.
For more information about learning how to live with cancer, read “Taking Time: Support for People With Cancer” from the National Cancer Institute. This booklet is available online at www.cancer.gov/cancertopics/takingtime.
Medications
Chemotherapy is the use of medicines to control the cancer’s growth or relieve symptoms. Often the medicines are given through a needle in your vein. Your blood vessels carry the medicines through your body. Sometimes the medicines are available as pills. And sometimes they are given as a shot, or injection.
Several medicines are used to treat colorectal cancer. There are also several medicines available for treating side effects.
Medicine choices
A combination of chemotherapy medicines often works better than a single drug in treating colorectal cancer. This may include medicines such as leucovorin, fluorouracil, and oxaliplatin.
Hair loss can be a common side effect with some types of chemotherapy. But hair loss usually isn’t a side effect of these drugs.
Treating the side effects
Your doctor may prescribe medicines that can help relieve side effects of chemotherapy. These side effects can include mouth sores, diarrhea, nausea, and vomiting. Your doctor may prescribe medicines to control nausea and vomiting.
There also are things you can do at home to manage side effects. See Home Treatment for more information.
What to think about
Chemotherapy and radiation may be combined to treat some types of colorectal cancer. Radiation or chemotherapy given before or after surgery can destroy microscopic areas of cancer to increase the chances of a cure.
Surgery
Surgery to remove cancer is almost always the main treatment for colorectal cancer. The type of surgery depends on the size and location of your cancer.
Side effects are common after surgery. You may be able to reduce the severity of your side effects at home. See Home Treatment for more information.
Surgery choices
- Polypectomy. When colorectal cancer is discovered in its very early stages, it can be removed during a sigmoidoscopy or colonoscopy. The surgeon cuts out not just the polyp, but also a small amount of tissue around it. The surgeon does not need to cut into the abdomen.
- Bowel resection. This involves cutting out the cancer as well as the sections of the colon or rectum that are next to it. Then the two healthy ends of the colon or rectum are sewn back together. This surgery is used when the cancer is larger. It can be done in two ways:
- Open resection. The surgeon makes a long cut (incision) in the belly, completes the bowel resection, and closes the incision.
- Laparoscopic surgery. This is done with several small incisions in the belly for a tiny camera and special tools. But laparoscopic surgery can’t always be done, such as when the cancer has spread to areas outside the colon.
Your doctor may suggest radiation therapy or chemotherapy if he or she thinks the cancer may come back (recur). If the cancer has spread to nearby lymph nodes, you may need chemotherapy after your surgery. Or if your surgery shows that the cancer has spread outside your colon or rectum, you may need radiation therapy.
What to think about
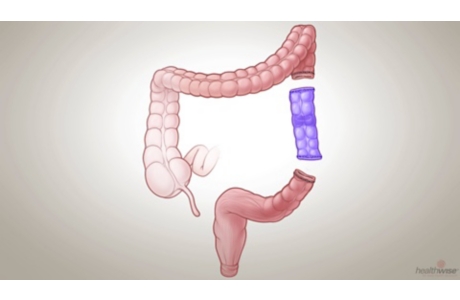
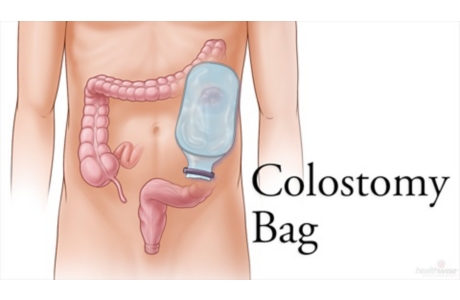
Sometimes after a bowel resection, the two ends of the colon or rectum can’t be sewn back together. When this happens, a colostomy is performed. But most people don’t need a colostomy.
Other Treatment
Radiation therapy
Radiation therapy uses X-rays to destroy colorectal cancer cells and shrink tumors. It is often used to treat rectal cancer, usually combined with surgery. It is used less often to treat colon cancer. It may also be combined with chemotherapy.
Radiation may be given:
- Externally, using a machine outside the body that points a beam of radiation at the tumor.
- Internally, by placing tiny radioactive “seeds” next to or into the cancer.
Compared to surgery alone, radiation given before surgery may reduce the risk that rectal cancer will return, and it may help you live longer.footnote 5
Complementary therapies
People sometimes use complementary therapies along with medical treatment to help relieve symptoms and side effects of cancer treatments. Some of the complementary therapies that may be helpful include:
- Acupuncture to relieve pain.
- Meditation or yoga to relieve stress.
- Massage and biofeedback to reduce pain and ease tension.
- Breathing exercises for relaxation.
Mind-body treatments like the ones listed above may help you feel better. They can make it easier to cope with cancer treatments. They also may reduce chronic low back pain, joint pain, headaches, and pain from treatments.
Before you try a complementary therapy, talk to your doctor about the possible value and side effects. Let your doctor know if you are already using any of these therapies. Complementary therapies are not meant to take the place of standard medical treatment. But they may improve your quality of life and help you deal with the stress and side effects of cancer treatment.
Clinical trials
You may be interested in taking part in research studies called clinical trials. Clinical trials are based on the most up-to-date information. They are designed to find better ways to treat people who have cancer. People who don’t want standard treatments or aren’t cured by standard treatments may want to take part in clinical trials. These are ongoing in most parts of the United States and in some other countries around the world for all stages of colorectal cancer.
References
Citations
- National Cancer Institute (2017). SEER cancer stat facts: Colon and rectum cancer. National Cancer Institute. https://seer.cancer.gov/statfacts/html/colorect.html. Accessed November 10, 2017.
- Winawer S, et al. (2003). Colorectal cancer screening and surveillance: Clinical guidelines and rationale—Update based on new evidence. Gastroenterology, 124(2): 544–560.
- Lewis C (2007). Colorectal cancer screening, search date November 2006. Online version of BMJ Clinical Evidence: http://www.clinicalevidence.com.
- U.S. Preventive Services Task Force (2016). Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. JAMA, 315(23): 2564–2575. DOI:10.1001/jama.2016.5989. Accessed June 27, 2016.
- Lewis C (2007). Colorectal cancer screening, search date November 2006. Online version of BMJ Clinical Evidence: http://www.clinicalevidence.com.
Other Works Consulted
- National Cancer Institute (2010). Colon Cancer PDQ: Treatment—Health Professional Version. Available online: http://www.cancer.gov/cancertopics/pdq/treatment/colon/HealthProfessional.
- National Cancer Institute (2011). Colon Cancer PDQ: Treatment—Patient Version. Available online: http://www.cancer.gov/cancertopics/pdq/treatment/colon/Patient.
- National Cancer Institute (2011). Rectal Cancer PDQ: Treatment—Health Professional Version. Available online: http://www.cancer.gov/cancertopics/pdq/treatment/rectal/HealthProfessional/allpages.
- National Cancer Institute (2012). Genetics of Colorectal Cancer PDQ—Health Professional Version. Available online: http://www.cancer.gov/cancertopics/pdq/genetics/colorectal/healthprofessional/allpages.
- National Cancer Institute (2012). Rectal Cancer Treatment (PDQ)—Patient Version. Available online: http://www.cancer.gov/cancertopics/pdq/treatment/rectal/Patient.
- National Comprehensive Cancer Network (2012). Rectal cancer. NCCN Clinical Practice Guidelines in Oncology, version 3. Available online: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp#site.
Current as of: December 19, 2018
Author: Healthwise Staff
Medical Review:E. Gregory Thompson MD – Internal Medicine & Kathleen Romito MD – Family Medicine & Kenneth Bark MD – General Surgery, Colon and Rectal Surgery & Adam Husney MD – Family Medicine
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.