Prostate Cancer
Overview
What is prostate cancer?
Prostate cancer is the abnormal growth of cells in a man’s prostate gland. The prostate sits just below the bladder. It makes part of the fluid for semen. In young men, the prostate is about the size of a walnut. As men age, the prostate usually grows larger.
Prostate cancer is common in men older than 65. It usually grows slowly and can take years to grow large enough to cause any problems. As with other cancers, treatment for prostate cancer works best when the cancer is found early. Often, prostate cancer that has spread responds to treatment. Older men who have prostate cancer usually die from other causes.
Experts don’t know what causes prostate cancer, but they believe that your age, family history (genetics), and race affect your chances of getting it.
What are the symptoms?
Prostate cancer usually doesn’t cause symptoms in its early stages. Most men don’t know they have it until it is found during a regular medical exam.
When problems are noticed, they are most often problems with urinating. But these same symptoms can also be caused by an enlarged prostate (benign prostatic hyperplasia). An enlarged prostate is common in older men.
See your doctor for a checkup if:
- You have urinary problems, such as:
- Not being able to urinate at all.
- Having a hard time starting or stopping the flow of urine.
- Having to urinate often, especially at night.
- Having pain or burning during urination.
- You have difficulty having an erection.
- You have blood in your urine or semen.
- You have deep and frequent pain in your lower back, belly, hip, or pelvis.
How is prostate cancer diagnosed?
The most common way to check for prostate cancer is to have a prostate-specific antigen (PSA) blood test. A higher level of PSA may mean that you have prostate cancer. But it could also mean that you have an enlargement or infection of the prostate.
If your PSA is high, you may need a prostate biopsy to figure out the cause. A biopsy means that your doctor takes tissue samples from your prostate gland and sends them to a lab for testing.
How is prostate cancer treated?
Your treatment will depend on what kind of cancer cells you have, how far they have spread, your age and general health, and your preferences.
You and your doctor may decide to manage your cancer with active surveillance or to treat it with surgery or radiation.
If you are over age 80 or have other serious health problems, like heart disease, you may choose not to have treatments to cure your cancer. Instead, you can just have treatments to manage your symptoms. This is called watchful waiting.
Choosing treatment for prostate cancer can be confusing. Talk with your doctor to choose the treatment that’s best for you.
How can treatment affect your quality of life?
Your age and overall health will make a difference in how treatment may affect your quality of life.
Both surgery and radiation can cause side effects. Radiation is more likely to cause bowel problems. Surgery is more likely to cause leaking urine or erection problems.
Medicines and mechanical aids may help men who have erection problems after surgery. And there are ways to target the radiation and protect the rectum during radiation.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Cause
The exact cause of prostate cancer isn’t known. But experts believe that your age and family history (genetics) may have something to do with your chances of getting the disease.
The prostate usually gets larger as you age. Having an enlarged prostate (benign prostatic hyperplasia, or BPH) is very common among older men and doesn’t increase your chances of getting prostate cancer. But an enlarged prostate is sometimes caused by prostate cancer instead of BPH.
Symptoms
Prostate cancer usually doesn’t cause symptoms in its early stages. When there are symptoms, they may include:
- Urinary problems, such as:
- Not being able to urinate at all.
- Having a hard time starting or stopping the flow of urine.
- Having to urinate often, especially at night.
- Having pain or burning during urination.
- Difficulty having an erection.
- Blood in your urine or semen.
- Deep and frequent pain in your lower back, belly, hip, or pelvis.
Symptoms that may show that the cancer has spread, or metastasized, to other parts of the body include:
- Weight loss.
- Bone pain, especially in the lower abdomen, hip, pelvis, or lower back.
- Swelling in the legs and feet.
For more information about prostate cancer that has come back or spread, see the topic Prostate Cancer, Advanced or Metastatic.
What Happens
Prostate cancer is a common cancer affecting older men. It usually takes years to become large enough to cause any problems. Sometimes, though, it grows quickly.
Many prostate cancers are found early, when the cancer cells are only in the prostate. When prostate cancer spreads beyond the prostate, it goes first to the lymph nodes in the pelvis, and then on to the bones, lungs, or other organs. For more information, see the topic Prostate Cancer, Advanced or Metastatic.
About 12 out of 100 men in the U.S. will be diagnosed with prostate cancer sometime during their lifetime.footnote 1 But most men who are diagnosed with prostate cancer don’t die from prostate cancer.
What Increases Your Risk
Some things can increase your chances of getting prostate cancer. These things are called risk factors. But many people who get prostate cancer don’t have any of these risk factors. And some people who have risk factors don’t get this cancer.
Age
Being older than 50 is the main risk factor for prostate cancer. About 6 out of 10 new prostate cancers are found in men who are 65 or older.footnote 2
Family history
Your chances of getting the disease are higher if other men in your family have had it.
- Your risk is doubled if your father or brother had prostate cancer. Your risk also depends on the age at which your relative was diagnosed.
- Men whose families carry the gene changes that cause breast cancer, BRCA1 or BRCA2, are thought to be at increased risk for prostate cancer.
Race
- Prostate cancer is more common among African-American men than men of other races. African-American men also have a greater chance of getting the kind of prostate cancer that grows and spreads.
- In men of other races, non-Hispanic white men are more likely to get prostate cancer than Hispanic or Asian-American men.
When To Call a Doctor
Call your doctor right away if:
- You cannot urinate.
- You have symptoms of a urinary infection. For example:
- You have blood or pus in your urine.
- You have pain in your back just below your rib cage.
- You have a fever, chills, or body aches.
- It hurts to urinate.
- You have groin or belly pain.
- You have pain in your back or hips.
- Your pain isn’t controlled.
- You are vomiting or nauseated.
Watch closely for changes in your health, and be sure to contact your doctor if:
- You have pain when you ejaculate.
- You have trouble starting or controlling your urine.
Who to see
The following health professionals can evaluate urinary symptoms:
The following doctors treat prostate cancer:
You may want to get a second opinion from a different specialist before making your treatment decision. For example, if your doctor is a family medicine physician, you may want to talk to a radiation oncologist, a urologist, or a urologic or medical oncologist.
Exams and Tests
Tests before diagnosis
Tests include:
- A digital rectal exam, in which the doctor inserts a gloved finger into your rectum to feel your prostate gland. Some prostate tumors can be found this way.
- A PSA test to measure the levels of prostate-specific antigen (PSA) in your blood. A higher level of PSA may be a sign of an enlargement, infection, or cancer of the prostate. If it’s possible that an infection is raising your PSA, you may first have 4 to 6 weeks of antibiotics. Your doctor may suggest a second PSA test before thinking about doing a biopsy.
- An MRI called a multiparametric MRI (mpMRI). It shows a picture of the prostate along with other important information, such as the size of the prostate, blood flow, and what the prostate tissue looks like.
- A transrectal ultrasound, in which the doctor inserts a probe into your rectum to check your prostate. The probe uses sound waves (ultrasound) to create a picture of the prostate.
- A tumor marker (biomarker) test, such as 4Kscore, the Mi-Prostate Score (MiPS), or the Prostate Health Index (PHI). These tests look for signs of cancer in a sample of blood or urine.
- A prostate biopsy, in which tissue is taken from the prostate and examined under a microscope. A biopsy is the only way to confirm whether you have prostate cancer.
Tests after diagnosis
If you have low-risk localized prostate cancer and decide on active surveillance, you will have regular checkups and tests, including PSA tests and prostate biopsies. You may also have other tests, such as an mpMRI. If there is no change in your condition, you may continue active surveillance. If tests show that your cancer is growing, you will need to consider having other treatment. Of course, you can also decide at any time to have treatment even if your cancer isn’t growing.
If your cancer appears to be a faster-growing type, more tests will be done to see if the cancer has spread. Tests may include:
Tests after treatment
After treatment for prostate cancer, you have regular checkups to check for any signs that the cancer has come back or spread. Tests include:
- Blood tests. Different types of blood tests are used to see whether cancer has spread to your bones or liver.
- A bone scan to check for bone damage caused by the cancer spreading.
- A CT scan or MRI to look for a new tumor.
Screening tests
Screening for prostate cancer involves checking for signs of the disease when there are no symptoms. It may be done with the PSA test. And while it’s important to have regular health checkups, experts disagree on whether PSA testing should be used to routinely screen men for prostate cancer. Testing could lead you to have cancer treatments that you don’t need.
So talk with your doctor. Ask about your risk for prostate cancer, and discuss the pros and cons of PSA testing.
Treatment Overview
Your treatment decision will depend on:
- Your age.
- Any serious health problems.
- Your PSA level.
- What kind of cancer cells you have. This is called the grade or Gleason score of your cancer. Most prostate cancer cells grow very slowly. But some types of cells grow quickly and spread to other areas of the body.
- How far your cancer has spread. This is called the stage of your cancer.
- The side effects of treatment.
- Your personal feelings and concerns.
Treatment may be more successful if prostate cancer is found and treated early. But not all prostate cancers may need to be treated, at least not right away. Treating low-risk prostate cancer may be unnecessary, as some of these cancers grow so slowly that they will never cause problems during a man’s lifetime. Unlike many other cancers, prostate cancer is usually slow-growing. For most men, this slow growth means they have time to learn all they can before deciding whether to have treatment or which treatment to have.
Types of treatment
The main treatments for prostate cancer include:
- Surgery to remove the cancer by removing the prostate gland. This operation is called a prostatectomy.
- Radiation treatments, which include external and internal radiation. These treatments have been improved with newer technologies that reduce side effects and other problems caused by radiation. To learn more, see Other Treatment.
Cancer that hasn’t spread outside the prostate is called localized prostate cancer. Men with localized prostate cancer have options for their care. Tests show if a localized prostate cancer is likely to grow.
- Low-risk means that the cancer isn’t likely to grow right away. Men have the option to choose active surveillance. This means their cancer will be watched closely by their doctors with regular checkups and tests to see if the cancer grows. This choice allows them to delay having surgery or radiation, often for many years. If the cancer grows very slowly, they may never need treatment.
- Medium-risk means that the cancer is more likely to grow. Some men may have the option to choose active surveillance. Most men will likely need treatment with surgery or radiation.
- High-risk means that the cancer will most likely grow right away. Men will likely need treatment with surgery or radiation.
Men who have prostate cancer that has come back or has already spread throughout the body may have other treatments, including hormone therapy.
A diagnosis of prostate cancer usually means that you will be seeing your doctor regularly for years to come. So it’s a good idea to build a relationship that is based on full and honest information. Ask your doctor questions about your cancer so that you can make the best decision about treatment. Your doctor also may give you some advice on changes to make in your life to help your treatment succeed.
Additional information about prostate cancer is provided by the National Cancer Institute at www.cancer.gov/cancertopics/types/prostate.
Side effects of treatment
Treatments such as surgery or radiation can cause serious side effects. Some are short-term problems. But a side effect can become a long-term problem.
- Surgery can cause leaking urine (urinary incontinence) and erection problems.
- Radiation can cause bowel problems, such as rectal pain, diarrhea, blood in your stool, and rectal leakage. It can also cause bladder problems, such as a burning feeling when you urinate.
For men with high-risk prostate cancer, radiation treatment is given along with hormone therapy. Hormone therapy has side effects, such as the loss of bone density and muscle mass. It can also increase the risk for bone fractures, diabetes, and heart disease.
In the first 2 to 5 years after treatment, the chance of having erection or bladder problems is higher with surgery. And the chance of having bowel problems, such as an urgent need to move your bowels, is higher with radiation. But at 15 years, the chance of erection, bladder, or bowel problems is about the same with either treatment.footnote 3
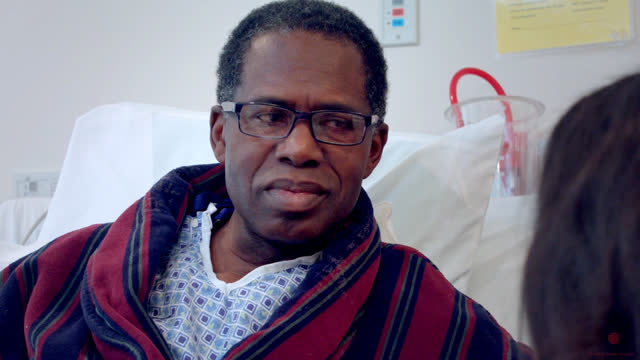
Coping with cancer
A cancer diagnosis can change your life. You may feel like your world has turned upside down and you have lost all control. Talking with family, friends, or a counselor can really help. Ask your doctor about support groups. Or call the American Cancer Society (1-800-227-2345) or visit the website at www.cancer.org.
Follow-up care
After surgery or radiation
If you choose surgery or radiation to treat your prostate cancer, it will be important to have regular checkups. If your cancer comes back, this will help your doctor find it early.
Treatment decisions
To make the decision that is best for you, take the time to understand your options and the medical facts about your cancer. Sometimes the medical facts will guide your decision. But a good decision also reflects what matters most to you. This includes how you feel about radiation or surgery and the likely side effects. It also includes deciding if you want any treatment if you are an older man or have other health problems.
- Age isn’t a reason to avoid surgery. But if you are 70 or older, other medical conditions, such as heart disease, may affect your decision. Men who are older also have a higher rate of incontinence and impotence after surgery. Age is especially important to think about if you have early-stage cancer, which generally grows slowly.
- Get a second or even a third opinion before making your treatment decisions. You may hear differing advice or opinions, which may seem confusing. But talking with other doctors can help you make your decision. If your doctor is a medical oncologist, you may want to talk with other prostate cancer specialists, such as a urologist, a radiation or urologic oncologist, or a surgeon.
- Studies show that fewer side effects are reported at large medical centers, where the surgeons do prostatectomies more often and so are more experienced and skilled.footnote 4
Prevention
One thing you can do that may lower the risk for prostate cancer is to eat some of these foods:
- Soy products, like tofu and soy beans.
- Tomatoes and foods that contain tomato sauce.
- Vegetables like broccoli, cauliflower, and cabbage.
- Fish, like salmon, albacore tuna, and sardines.
- Walnuts and flaxseed, and their oils.
Being physically active and staying at a healthy body weight also can help reduce the risk of prostate cancer.footnote 5
Home Treatment
Managing symptoms and side effects
During any stage of prostate cancer, there are things you can do at home to help manage the symptoms of cancer or the side effects of treatment or both. If your doctor has given you instructions or medicines to treat symptoms or side effects, be sure to use them. Healthy habits such as eating right and getting enough sleep and exercise can help control your symptoms and side effects.
Try the following tips to manage:
- Nausea or vomiting. Watch for and treat early signs of dehydration, such as having a dry mouth or feeling lightheaded when you stand up. Eating smaller meals may help. So can a little bit of ginger candy or ginger tea.
- Pain. Not all forms of cancer or cancer treatment cause pain. But if you do have pain, there are many home treatments that can help.
- Diarrhea. Rest your stomach, and be alert for signs of dehydration. Check with your doctor before using any nonprescription medicines for your diarrhea. Be sure to drink enough fluids.
- Constipation. Make sure you drink enough fluids and eat fruits, vegetables, and fiber in your diet each day. Do not use a laxative without first talking to your doctor.
- Sleep problems. Often, simple measures such as having a regular bedtime, getting some exercise during the day, and having no caffeine late in the day can help with sleep problems.
- Urinary problems. Home treatment for urinary incontinence includes eliminating caffeinated drinks from your diet and setting a schedule of urinating every 3 to 4 hours, regardless of whether you feel the need. Try doing pelvic floor (Kegel) exercises to strengthen your pelvic muscles.
Managing stress
- Learning that you have prostate cancer and being treated for it can be very stressful. Find ways to reduce your stress.
- You may want to talk with family or friends. Some people find that spending time alone is what they need. Consider meeting with a counselor or joining a support group of others who have prostate cancer.
- Your doctor may also be able to help you find other sources of support and information. Learning relaxation techniques, such as yoga or visualization exercises, may also help you reduce your stress. Your feelings about your body may change after treatment. Dealing with your body image may involve talking openly about your worries with your partner and discussing your feelings with a doctor.
For more information, see the topic Getting Support When You Have Cancer.
Medications
Hormones are medicines that can affect the growth of prostate cancer cells. Hormone therapy is sometimes used with radiation treatment or surgery to help make sure that all cancer cells are destroyed.
Hormone therapy can’t cure prostate cancer. But it will usually shrink the tumor and slow the rate of cancer growth, sometimes for years. Taking a hormone-therapy medicine lowers your level of testosterone and other male hormones. Another way to lower male hormones is by having surgery to remove the testicles, called an orchiectomy.
Surgery
Surgery for prostate cancer may be done to:
- Remove the prostate and its cancer (prostatectomy). Nearby lymph nodes also may be removed to check for cancer (lymphadenectomy) during a prostatectomy.
- Fix urinary problems that are caused by a tumor pressing on the urethra (transurethral resection of the prostate, or TURP).
Radical prostatectomy
Radical prostatectomy is an operation to remove the entire prostate and any nearby tissue that may contain cancer. It can be done as open surgery through an incision (cut) in the belly, or as laparoscopic surgery through several very small incisions in the belly. Laparoscopic surgery to remove the prostate is done with a tiny camera and special tools. Sometimes lymph nodes in the area also are removed so that they can be checked for signs of cancer. This is called a lymph node biopsy.
- Nerve-sparing surgery helps preserve the nerves that are along the side of the prostate and that are needed for an erection. This is only done when there is little chance of leaving cancer cells behind. If you already have sexual function issues, nerve-sparing surgery may not be the best choice for you.
- Robotic-assisted laparoscopic radical prostatectomy is surgery done through small incisions in the belly with robotic arms that translate the surgeon’s hand motions into finer and more precise movements. This surgery requires specially trained doctors.
Surgery may completely remove your prostate cancer. But it isn’t possible to know for sure before surgery whether the cancer has spread beyond the prostate. When cancer has spread, it can’t always be cured with surgery alone.
Other Medical Treatment
Active surveillance or watchful waiting
Active surveillance means that you will be watched closely by your doctor. If the cancer starts to grow more quickly, you will need to have other treatment, such as surgery. Your regular checkups may include digital rectal exams, PSA tests, and biopsies.
Watchful waiting also means that you will be closely watched by your doctor. But the goal of watchful waiting is to treat symptoms that cause problems rather than to cure the cancer. Men who are older and men who have other serious health problems, like heart disease, and aren’t well enough to have surgery or radiation often choose watchful waiting.
Radiation therapy
Radiation therapy may be used alone or combined with hormone treatment when the cancer has high-risk features (based on Gleason score and stage). Radiation may also be used when the cancer has spread after surgery.
Radiation treatment for prostate cancer includes:
- External radiation. Also called external beam radiotherapy, or EBRT, radiation therapy uses high-energy rays, such as X-rays, to destroy the cancer. It is usually given in multiple doses over 4 to 9 weeks. Radiation destroys tissue, so it may damage the nerves along the side of the prostate that affect your ability to have an erection. If you already have bowel problems, external radiation may make your symptoms worse. The most common forms of external radiation are:
- Conformal radiotherapy (3D-CRT). It uses a three-dimensional planning system to target a strong dose of radiation to the prostate cancer. This helps to protect healthy tissue from radiation.
- Intensity-modulated radiation therapy (IMRT). It uses newer 3D-CRT technology to target the cancer.
- Proton beam therapy. This is radiation therapy that uses a different type of energy (protons) rather than X-rays. This allows a higher amount of specifically directed radiation, which protects nearby healthy tissues (especially the rectum). Sometimes proton beam therapy is combined with X-ray therapy. (It is available only at big medical centers.)
- Internal radiation (brachytherapy). Brachytherapy is a one-time radiation treatment that uses tiny radioactive seeds. After you are given anesthesia, the doctor uses a needle to inject the seeds into your prostate, where they slowly release radiation directly into the cancer. Sometimes external radiation or hormone therapy is added to brachytherapy. If you already have urinary problems, brachytherapy may make your symptoms worse.
- High-dose-rate (HDR) brachytherapy. For this form of brachytherapy, radioactive material is placed into the prostate for a very brief period of time (seconds to minutes) and then removed. The radiation is delivered this way several times.
Less common or newer treatments
Some less common or newer treatments still being studied for prostate cancer include:
- Cryosurgery. This treatment freezes the prostate gland to kill the cancer.
- High-intensity focused ultrasound (HIFU). This treatment uses sound waves to destroy prostate tissue.
- MRI-guided focal laser ablation. This treatment uses heat from a laser to destroy prostate tissue.
Clinical trials
Your doctor may talk to you about joining a research study called a clinical trial if one is available in your area. Clinical trials are research studies to look for ways to improve treatments for prostate cancer.
Complementary therapy
People sometimes use complementary therapies along with medical treatment to help relieve symptoms and side effects of cancer treatments. Some of the complementary therapies that may be helpful include:
- Acupuncture to relieve pain. Acupuncture may also help reduce hot flashes from taking hormone therapy.
- Meditation or yoga to relieve stress.
- Massage and biofeedback to reduce pain and ease tension.
- Breathing exercises for relaxation.
Mind-body treatments like those mentioned above may help you feel better and cope better with treatment. These treatments also may reduce chronic low back pain, joint pain, headaches, and pain from treatments.
Before you try a complementary therapy, talk to your doctor about the possible value and potential side effects. Let your doctor know if you are already using any such therapies. Complementary therapies aren’t meant to take the place of standard medical treatment. But they may improve your quality of life and help you deal with the stress and side effects of cancer treatment.
References
Citations
- National Cancer Institute (2017). SEER cancer stat facts: Prostate cancer. National Cancer Institute. www.seer.cancer.gov/statfacts/html/prost.html. Accessed July 10, 2017.
- American Cancer Society (2012). Cancer Facts and Figures 2012. Atlanta: American Cancer Society. Available online: http://www.cancer.org/Research/CancerFactsFigures/CancerFactsFigures/cancer-facts-figures-2012.
- Resnick MJ, et al. (2013). Long-term functional outcomes after treatment for localized prostate cancer. The New England Journal of Medicine, 368(5): 436–445.
- Rosenberg JE, Kantoff PW (2011). Prostate cancer. In EG Nabel, ed., ACP Medicine, section 12, chap. 9. Hamilton, ON: BC Decker.
- Kushi LH, et al. (2012). American Cancer Society guidelines on nutrition and physical activity for cancer prevention. CA: A Cancer Journal for Clinicians, 62: 30–67.
Other Works Consulted
- Keating NL, et al. (2010). Diabetes and cardiovascular disease during androgen deprivation therapy: Observational study of veterans with prostate cancer. Journal of the National Cancer Institute, 102(1): 39–46.
- Malcolm JB, et al. (2010). Quality of life after open or robotic prostatectomy, cryoablation or brachytherapy for localized prostate cancer. Journal of Urology, 183(5): 1822–1828.
- National Cancer Institute (2011). Prostate Cancer Treatment (PDQ)—Patient Version. Available online: http://www.cancer.gov/cancertopics/pdq/treatment/prostate/patient.
- National Comprehensive Cancer Network (2012). Prostate cancer. NCCN Clinical Practice Guidelines in Oncology, version 2.2012. Available online: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.
- Pagana KD, Pagana TJ (2010). Mosby’s Manual of Diagnostic and Laboratory Tests, 4th ed. St. Louis: Mosby Elsevier.
- Schaeffer EM, et al. (2012). Radical retropubic and perineal prostatectomy. In AJ Wein et al., eds., Campbell-Walsh Urology, 10th ed., vol. 3, pp. 2801–2829. Philadelphia: Saunders.
- Scher HI, et al. (2015). Cancer of the prostate. In VT DeVita Jr et al., eds., DeVita, Hellman, and Rosenberg’s Cancer Principles and Practices of Oncology, 10th ed., pp. 932–980. Philadelphia: Walters Kluwer.
- Su L, Smith JA (2012). Laparoscopic and robotic-assisted laparoscopic radical prostatectomy and pelvic lymphadenectomy. In AJ Wein et al., eds., Campbell-Walsh Urology, 10th ed., vol. 3, pp. 2830–2849. Philadelphia: Saunders.
Current as of: December 19, 2018
Author: Healthwise Staff
Medical Review:E. Gregory Thompson MD – Internal Medicine & Kathleen Romito MD – Family Medicine & Adam Husney MD – Family Medicine & Christopher G. Wood MD, FACS – Urology, Oncology & Richard M. Hoffman MD, MPH – Internal Medicine
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.