Type 2 Diabetes in Children
Topic Overview
Is this topic for you?
This topic provides information about type 2 diabetes in children. If you are looking for information about type 1 diabetes, see the topic Type 1 Diabetes: Children Living With the Disease.
What is type 2 diabetes?
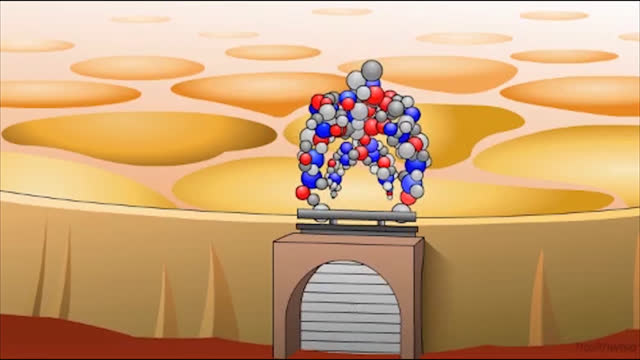
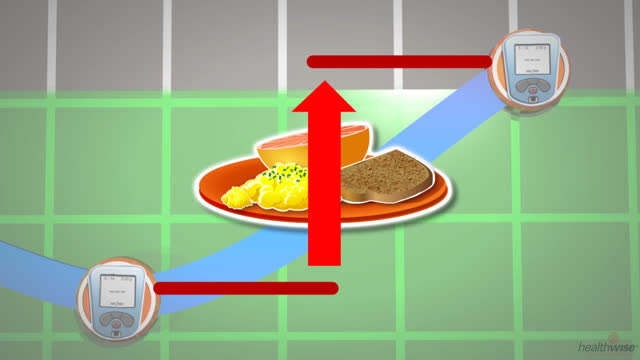
Type 2 diabetes is a disease that develops when the body’s tissues cannot use insulin properly. Over time, the pancreas cannot make enough insulin. Insulin is a hormone that helps the body’s cells use sugar (glucose) for energy. It also helps the body store extra energy in muscle, fat, and liver cells.
Without insulin, the sugar cannot get into the cells to do its work. It stays in the blood instead. This can cause high blood sugar levels. A person has diabetes when the blood sugar stays too high too much of the time.
High blood sugar can cause problems with the eyes, heart, blood vessels, nerves, and kidneys. High blood sugar also makes a person more likely to get serious illnesses or infections.
In the past, doctors believed that type 2 diabetes was an adult disease and that type 1 diabetes was a children’s disease. Now, more and more children are getting type 2 diabetes.
Finding out that your child has diabetes can be scary. But your child can live a long, healthy life by learning to manage the disease.
What causes type 2 diabetes?
Doctors do not know exactly what causes diabetes. Experts believe the main risks for children getting type 2 diabetes are being overweight, not being physically active, and having a family history of the disease.
Also, the hormones released during the early teen years make it harder than usual for the body to use insulin correctly. This problem is called insulin resistance. It can lead to diabetes.
What are the symptoms?
Most children with type 2 diabetes do not have symptoms when the disease is first found. If there are symptoms, they usually are mild and may include:
- Having to urinate more often.
- Feeling a little more thirsty than normal.
- Losing a little weight for no clear reason.
How is type 2 diabetes diagnosed?
A simple blood test is usually all that is needed to diagnose diabetes. Your child’s doctor may do other blood tests if it is not clear whether your child has type 1 or type 2 diabetes.
A doctor may test your child for diabetes if he or she is overweight, gets little physical activity, or has other risk factors for the disease. A risk factor is anything that increases your chances of having a disease. Some children are diagnosed with type 2 diabetes when they have a blood or urine test for some other reason.
How is it treated?
The key to treating diabetes is to keep your child’s blood sugar levels within a target range. To do this:
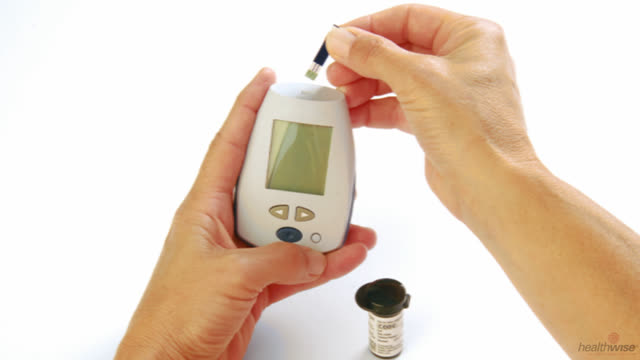
- Keep track of your child’s blood sugar levels. This will help you and your child learn how different foods and activities affect his or her blood sugar. Your doctor can teach you and your child how to do this.
- Teach your child to make healthy food choices.
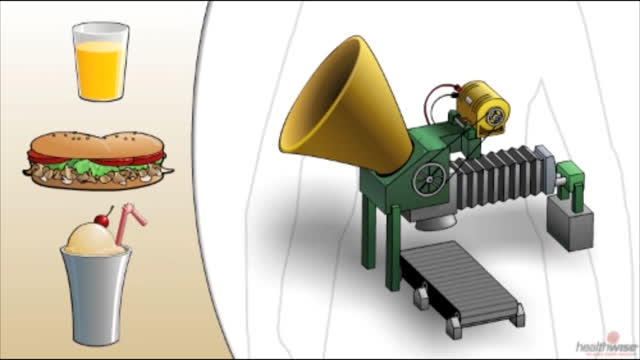
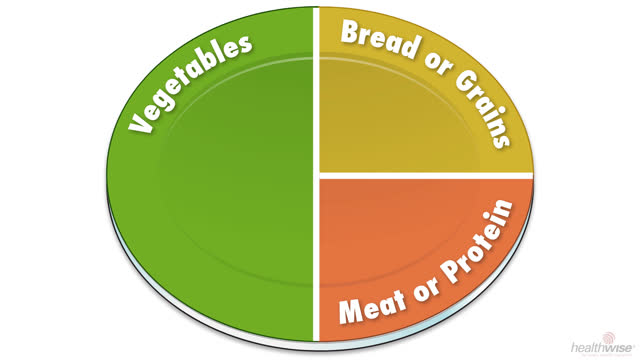
- Help your child to eat about the same amount of carbohydrates at each meal. This helps keep your child’s blood sugar steady. Carbohydrates affect blood sugar more than other nutrients. It is found in sugar and sweets, grains, fruit, starchy vegetables, and milk and yogurt.
- Talk to your doctor, a diabetes educator, or a dietitian about an eating plan that will work for your child. There are many ways to manage how much and when your child eats.
- Help your child stay active. Your child does not have to start a strict exercise program, but being more active can help control blood sugar. For example, your child could play outside with friends, take walks with family members, or take part in sports.
- Set a good example. It will be easier for your child if the rest of the family also eats well and gets regular exercise. This may also reduce the risk that other family members will get the disease.
- If your child needs medicine for diabetes, make sure that he or she takes it as prescribed.
You play a major role in helping your child take charge of his or her diabetes care. Let your child do as much of the care as possible. At the same time, give your child the support and guidance he or she needs.
The longer a person has diabetes, the more likely he or she is to have problems, such as diseases of the eyes, heart, blood vessels, nerves, and kidneys. But if your child can control his or her blood sugar levels every day, it may help to delay the start of or prevent some of these problems later on.
Even when you are careful and do all the right things, your child can have problems with high or low blood sugar. It is important to know what signs to look for and what to do if this happens.
Can type 2 diabetes be prevented?
Helping your child stay at a healthy weight and get regular exercise can help prevent type 2 diabetes.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
- Diabetes in Children: Checking Blood Sugar in a Child
- Diabetes in Children: Counting Carbs
- Diabetes in Children: Giving Insulin Shots to a Child
- Diabetes in Children: Preparing a Care Plan for School
- Diabetes in Children: Preventing High Blood Sugar
- Diabetes in Children: Treating Low Blood Sugar
- Healthy Eating: Helping Your Child Learn Healthy Eating Habits
Cause
The exact cause of type 2 diabetes is not known. But experts believe the disease develops in children the same way it does in adults. The body cannot correctly use the hormone insulin that is available. This is called insulin resistance. Over time, the pancreas does not produce enough of the hormone insulin.
Things that affect the body’s resistance to insulin in childhood include:
- Developmental stage. Growth hormone released during puberty can make it harder than usual for the body to use insulin correctly.
- Being female. Girls seem to develop more resistance to insulin than boys.
- Race. Hispanic, African-American, Native American, Asian-American, or Pacific Island ancestry raises risk for type 2 diabetes.
- Body composition. Insulin resistance increases as the amount of fat around the waist increases.
- Activity. Exercise may improve how the body’s cells use insulin and get the sugar they need.
Symptoms
Children often have no symptoms of type 2 diabetes before they are diagnosed, because their blood sugar level has been rising so slowly. As a result, a child may have diabetes for several months or years before being diagnosed.
When children do have symptoms, the most common include:
- Slight increase in the frequency of urination. Your child may have started wetting the bed at night.
- Slight increase in thirst.
Other possible symptoms include:
- Increased tiredness.
- Nausea.
- Blurred vision.
- Frequent infections and slow-healing wounds or sores.
- Weight loss.
What Happens
Type 2 diabetes usually develops in adulthood, but the number of children being diagnosed with the disease is rising. Children with type 2 diabetes are usually diagnosed during the early teen years. During this time, their bodies are growing and developing rapidly, placing a demand on the pancreas to produce additional insulin.
The hormones released during puberty can make it harder than usual for the body to use insulin correctly (insulin resistance). Also, children with type 2 diabetes are usually overweight, which also contributes to insulin resistance. If the pancreas cannot produce enough insulin to overcome the resistance, diabetes can develop.
Diabetes experts believe the disease progresses as it does in adults. The main risk factors for complications from diabetes are the length of time a person has diabetes and the degree of blood sugar control. A child who develops type 2 diabetes may have an increased risk of complications, because he or she will have the disease for a long time. Some complications that children and teens may develop include:
- Eye disease (diabetic retinopathy) and kidney disease (diabetic nephropathy).
- High blood pressure or high cholesterol, which increases the risk of heart and blood vessel disease later in life.
If a child’s blood sugar levels remain high for a long time, he or she may grow at an abnormal rate—faster than normal for a while, then slower than normal later. If blood sugar levels stay high during puberty, normal changes and the start of menstruation may be delayed.
The way to prevent complications is to always keep blood sugar levels in a target range. This requires that your child follow his or her treatment plan daily and monitor blood sugar levels often. Your child also will need ongoing diabetes education and regular checkups. Other medical conditions, such as high blood pressure and high cholesterol, need adequate medical care also, because they raise the risk for diabetes complications.
Children with type 2 diabetes have to modify their lifestyles. Your child will be more successful if your whole family is involved. These lifestyle changes benefit everyone by reducing the risk for diabetes and heart disease.
What Increases Your Risk
The major risk factors for type 2 diabetes in children include:
- Being overweight.
- Getting little or no physical activity.
- Having a parent, sister, or brother with the disease.
Other things that increase risk include:
- Race. African-American, Hispanic, Native American, Asian-American, and Pacific Islander children are at greater risk for type 2 diabetes than white American children.
- The child’s mother having diabetes that developed during pregnancy (gestational diabetes).
- The child being small for gestational age at birth.
Medical conditions that contribute to the risk of complications in adolescence and beyond include:
- High blood pressure.
- High cholesterol and high triglycerides.
- Fatty liver, in which fat is deposited in the liver.
- Sleep apnea, in which breathing stops briefly during sleep.
Teens who have diabetes and smoke have a higher risk of complications from diabetes than do those who do not smoke.
When should you call your doctor?
Call 911 or other emergency services right away if your child:
- Has symptoms of hyperosmolar state, such as:
- Blurred vision.
- Trouble staying awake or trouble being woken up.
- Fast, deep breathing.
- Breath that smells fruity.
- Belly pain, not feeling hungry, and vomiting.
- Feeling confused.
- Less common in type 2 diabetes is diabetic ketoacidosis (DKA), which has symptoms similar to those of hyperosmolar state. But DKA is still possible and very dangerous.
- Has passed out (lost consciousness) or has suddenly become very sleepy or confused. (Your child may have very low blood sugar, called hypoglycemia.)
Call a doctor if your child:
- Is sick and has blood sugar that cannot be controlled.
- Has been vomiting or has had diarrhea for more than 6 hours.
- Has blood sugar that stays higher than the level the doctor has set for your child, for example, 240 mg/dL for two or more readings.
- Has blood sugar that stays lower than the level the doctor has set for your child, for example, 70 mg/dL for two or more readings.
- Has symptoms of low blood sugar, such as:
- Sweating.
- Feeling nervous, shaky, and weak.
- Extreme hunger and slight nausea.
- Dizziness and headache.
- Blurred vision.
- Confusion.
Check with your doctor if your child:
- Often has problems with high or low blood sugar levels.
- Has trouble knowing when his or her blood sugar is low (hypoglycemia unawareness).
- Or you have questions or want to know more about diabetes.
Watchful waiting
Watchful waiting is a period of time during which you and your doctor observe your child’s symptoms or condition without using medical treatment. Watchful waiting is not appropriate if:
- You think your child may have symptoms of type 2 diabetes. A simple blood test is all that is needed to determine whether your child has the disease.
- Your child is overweight and gets little or no exercise. He or she is at risk for diabetes. Early detection and treatment for type 2 diabetes can prevent or delay complications from the disease.
- You have been told that your child has prediabetes. This condition can lead to type 2 diabetes. If your child eats a healthy diet and exercises regularly, he or she may not develop diabetes.
Who to see
Most doctors can diagnose diabetes. After your child has been diagnosed, your doctor will work with you to build a treatment plan that fits your child’s needs. Health professionals who may be involved in the treatment of children with type 2 diabetes include:
- A pediatrician, family medicine doctor, or general practitioner.
- A nurse practitioner or physician assistant.
- A pediatric endocrinologist.
- A certified diabetes educator (CDE). A CDE is a registered nurse, dietitian, doctor, pharmacist, or other health professional who has special training and experience in caring for people with diabetes.
- A registered dietitian, to help build a daily meal plan for your child and your family.
- A psychologist, to help with emotional or family issues that might affect treatment.
- An exercise specialist, to help your child and family plan a program of regular physical activity.
Exams and Tests
Many children have no symptoms before they are diagnosed with type 2 diabetes.
If a doctor suspects that your child may have type 2 diabetes, he or she will do a medical history, physical exam, and blood glucose testing. If the results of these tests meet the criteria for diagnosing diabetes established by the American Diabetes Association (ADA), your child has diabetes.
Other possible tests
If it is hard to tell whether your child has type 2 or type 1 diabetes, your doctor may do a C-peptide test or test for autoantibodies. (Autoantibodies are produced when the body’s immune system does not work right. These tests can help diagnose type 1 diabetes.)
Another form of diabetes, maturity onset diabetes of the young (MODY), is an inherited disease caused by a change (mutation) in a gene. There are many types of MODY depending on the gene that is affected. Genetic testing can help you and your doctor decide how to treat MODY.
Monitoring tests if diagnosed with diabetes
Because your child is at risk for diabetes complications (eye, heart, kidney, nerve, liver, and blood vessel problems), he or she needs to see a doctor regularly for tests to monitor type 2 diabetes.
Early detection
If your child is overweight and gets little or no exercise, he or she may be at risk for type 2 diabetes. Early detection and treatment for type 2 diabetes can prevent or delay problems from the disease.
Treatment Overview
Treatment of type 2 diabetes in children focuses on keeping blood sugar levels within a target range. Children may need higher blood sugar goals than adults, because their bodies are still developing. Also, they may not be able to recognize symptoms of low blood sugar. To reach his or her target blood sugar, your child needs to eat healthy meals of appropriate portion size and get daily exercise. Treatment also may include medicine.
Healthy eating
A healthy diet with the right amount of calories will help your child achieve target blood sugar levels and maintain a healthy weight. The meal plan designed for your child will spread carbohydrates (starches and sugary foods) throughout the day. This helps prevent high blood sugar after meals as well as weight gain. A registered dietitian can design a meal plan that not only fits your child’s needs but also is a healthy eating plan for your family. For more information, see the topic Healthy Eating for Children.
Weight management
If your child is overweight, he or she may need to lose weight (or stay at the same weight and not gain more). This depends on his or her age, development, and other risk factors.
Being physically active
Physical activity is extremely important. It helps the body use insulin correctly and helps control weight. Your child does not have to start a rigorous exercise program, but being more active can help control blood sugar. For example, your child could play outside with friends, take brisk walks with family members, and take part in individual or team sports.
Experts recommend that teens and children (starting at age 6) do moderate to vigorous activity at least 1 hour every day.footnote 1 And 3 or more days a week, what they choose to do should:
- Make them breathe harder and make the heart beat much faster.
- Make their muscles stronger. For example, they could play on playground equipment, play tug-of-war, lift weights, or use resistance bands.
- Make their bones stronger. For example, they could run, do hopscotch, jump rope, or play basketball or tennis.
It’s okay for them to be active in smaller blocks of time that add up to 1 hour or more each day.
Limit your child’s screen time. Have your child take breaks from computer, cell phone, and TV use and be active instead.
Medicines
Your child may need medicines if eating healthy meals and getting regular physical activity have not lowered your child’s blood sugar to his or her target level.
- Medicines for diabetes help the body produce more insulin, decrease the body’s resistance to insulin, or slow the absorption of carbohydrates from the intestine. Your child may need one medicine at some times and more than one at other times.
- Some children need daily insulin shots—alone or with other medicines. Even if your doctor does not prescribe daily insulin, your child may need to take insulin temporarily when first diagnosed or during illness or surgery. If the progression of diabetes cannot be stopped, your child eventually may need to take insulin daily.
Checking blood sugar, blood pressure, and cholesterol
Your child’s blood sugar level may need to be checked regularly, for example, before breakfast and 2 hours after meals.
If your child has high blood pressure or high cholesterol, those conditions need to be treated.
- High blood pressure is usually treated with angiotensin-converting enzyme (ACE) inhibitors or angiotensin ll receptor blockers (ARBs), because these medicines also protect the circulatory system and the kidneys from damage caused by diabetes. Sexually active teens should be warned that ACE inhibitors and ARBs should not be taken during pregnancy.
- Weight loss and well-controlled blood sugar can help lower your child’s cholesterol. Your child’s doctor may recommend medicine if these lifestyle changes do not lower cholesterol. Sexually active teens should be warned against becoming pregnant while taking these medicines.
What to think about
Some children have very high blood sugar levels when they are diagnosed with type 2 diabetes. A child with a very high blood sugar level may develop the serious chemical imbalance diabetic ketoacidosis and need to be treated with insulin in a hospital. After blood sugar returns to a target level, the child usually no longer needs insulin. His or her own body may start making enough insulin again.
Treating diabetes with medicine increases the risk for low blood sugar episodes. Your child’s doctor will determine the target range for your child’s blood sugar that will prevent damage from diabetes while causing as few low blood sugar episodes as possible.
The lifestyle changes needed to control diabetes can be especially hard for a child or teen. Your child will have a better chance of being successful if the whole family is involved. Eating a healthy diet and getting regular exercise may help other family members avoid diabetes.
Teens who have depression or an eating disorder may have difficulty keeping their blood sugar at a healthy level. Also, teens who smoke or use alcohol or other drugs have problems with blood sugar control. Support groups may help teens deal with diabetes management issues, which can improve the teens’ perception of diabetes care and blood sugar control.
Prevention
Healthy meals, physical activity, and weight control can help prevent diabetes or can prevent or delay complications if your child has diabetes. A registered dietitian can help you build a healthy meal plan for your child. Your doctor, exercise specialist, or certified diabetes educator also can help your child find ways to become more physically active.
Weight loss is appropriate if your child is overweight and he or she has reached adult height. In some severe cases, weight loss before your child reaches his or her full adult height may be needed. See the Interactive Tool: What Is Your Child’s BMI?
Having a blood sugar level that is higher than normal but not yet at the level of diabetes (prediabetes) increases a child’s risk for type 2 diabetes. If your child has prediabetes, eating a healthy diet and increasing physical exercise may make his or her blood sugar return to a normal range and possibly prevent type 2 diabetes. Your child will still need to see a doctor regularly to check for signs of the disease.
Home Treatment
Healthy eating
Your child needs to eat healthy meals with appropriate portions to support growth and prevent weight gain. The meal plan for your child will also spread carbohydrates throughout the day to prevent high blood sugar after meals. For information on healthy eating and weight management, see the topic Healthy Eating for Children.
Physical activity
Encourage your child (age 6 to 17) to do moderate to vigorous activity at least 1 hour every day. Limit the amount of time your child watches TV and uses the computer and cell phone. You can help your child or teen be active by looking for ways to make activity more fun and by being active along with your child.
For children age 2 to 5 years: The American Academy of Pediatrics advises parents to limit screen time to 1 hour a day or less. And it’s best for children younger than 2 to not watch TV, watch movies, or play games on a screen.
Work with your child’s teachers and school to make a plan to handle your child’s special needs, including testing blood sugar and eating snacks when needed.
Your child can take part in the same activities as other children. For safety:
- Let the coach know that your child has diabetes. If your child doesn’t take insulin, he or she may not be at risk for low blood sugar episodes. But making sure that the coach knows the symptoms of low blood sugar may still be a good idea.
- Take your child’s home blood sugar meter to sports practice sessions and games. Check his or her blood sugar level before and after each activity, if needed.
- Take a snack that contains carbohydrates to all practice sessions and games in case of a low blood sugar episode.
Home blood sugar monitoring
You and your child will need to monitor his or her blood sugar frequently to know how well it is under control. Talk with your doctor about a target range for your child. Young children may need a higher blood sugar goal than adults because of growth needs and to prevent very low blood sugar (hypoglycemia). As your child grows older, the goal can be lowered so that it is closer to the recommended target range.
Insulin injections
Your child may not need to take insulin if his or her blood sugar levels are staying within a target range with meal planning, exercise, and possibly other medicine. But at some point your child may need to take insulin because the pancreas may produce less and less insulin.
If your child takes insulin, you and your child need to know how to prepare and give a shot.
Other issues
Other important issues include:
- How to recognize and treat high blood sugar. Blood sugar levels that suddenly rise above a target range can lead to an emergency.
- How to recognize and treat low blood sugar. Your child is not likely to have a sudden drop in blood sugar level unless he or she is taking sulfonylurea or meglitinide medicines for diabetes or insulin injections and is unable to eat regular meals.
- Wearing medical identification at all times. In an emergency, medical identification lets people know that your child has diabetes so they can care for your child appropriately.
- Where to get support. Many areas of the country have support groups for children and teens with diabetes and for family members. These groups provide encouragement and suggestions that may help you and your child deal with the daily issues of diabetes care. Talk with your doctor about groups in your area.
- How to care for the feet. Your child needs to wear shoes that fit properly. He or she should not go barefoot outdoors if there is a risk of getting a cut or any foot injury. It’s a good idea to begin the habit of inspecting your child’s feet periodically or any time he or she has a foot complaint. Look for signs of injury or infection. If you notice a foot problem, even a minor one, talk with your doctor before treating it.
- What to do for illness. Some general sick-day guidelines may be helpful. These include checking your child’s blood sugar every 4 hours during the illness and encouraging your child to drink fluids to prevent dehydration. Do not give your child any nonprescription medicines without talking with a doctor or pharmacist. Some of these medicines can affect blood sugar levels.
What to think about
Childhood and the teen years are a difficult time to be diagnosed with diabetes. Normal developmental changes may interfere with your child following his or her treatment. Teens with diabetes may rebel against treatment or participate in risky behavior, such as using drugs or drinking alcohol.
You play a major role in helping your child become independent in his or her diabetes care. Allow your child to do as much of the care as possible. But give your child the support and guidance he or she needs. Your child will be more successful if your family is physically active and has healthy eating habits.
- Children in elementary school can cooperate in all tasks required for their care. By age 8, children can test their own blood sugar if they are supervised.
- Children in middle school or junior high school should be able to test their own blood sugar, but they may need help during low blood sugar episodes. By age 10, some children can give insulin injections if they are supervised.
- With appropriate supervision, teens should be able to handle their care. If the teen needs to take insulin, he or she may choose to use an insulin pump instead of injections. If your teen chooses to use a pump, be sure to supervise.
Medications
Medicine choices
Medicines that may be prescribed for children with type 2 diabetes are:
- Metformin.
-
This is the medicine of choice for children with type 2 diabetes. It is taken as a pill.
- Insulin.
-
Your doctor may suggest insulin if metformin doesn’t keep your child’s blood sugar in the target range. Insulin can be taken as a shot (injection) or through an insulin pump.
- Some children need daily insulin. Even if your doctor doesn’t prescribe daily insulin, your child may need to take it for a while when first diagnosed or during illness or surgery.
- Insulin may be given as a single nighttime dose, as several smaller doses throughout the day, or both.
Medicines to control blood pressure and cholesterol
Some children may need medicines to lower their blood pressure and cholesterol to reduce the risk for later complications.
- Angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) may be used to lower your child’s blood pressure.
- Statins may be used if a healthy diet and physical activity do not lower cholesterol. Sexually active teens should be warned against becoming pregnant while taking these medicines.
Surgery
When obesity is severe in older adolescents with type 2 diabetes, gastric bypass or other similar surgery may be considered as a last resort. For more information, see the topic Obesity.
Other Treatment
Children who have type 2 diabetes should not try to lose weight by following a fad diet or by enrolling in a quick-fix weight loss program. Most doctors recommend that children who are overweight eat a healthy diet that provides appropriate calories to prevent further weight gain.
Weight loss is appropriate if your child is overweight and he or she has reached adult height. In some severe cases, weight loss before your child reaches his or her full adult height may be needed.
Complementary medicine
Along with medical treatment, you may wonder if complementary therapies, especially dietary supplements, may help your child. There isn’t enough scientific evidence to say that any dietary supplement can prevent or manage type 2 diabetes.footnote 2
Talk with your doctor about any complementary health practice that you would like your child to try or your child is already using. Your doctor can help you manage your child’s health better if he or she knows about all of your child’s health practices.
References
Citations
- U.S. Department of Health and Human Services (2008). 2008 Physical Activity Guidelines for Americans (ODPHP Publication No. U0036). Washington, DC: U.S. Government Printing Office. Available online: http://www.health.gov/paguidelines/guidelines/default.aspx.
- National Center for Complementary and Integrative Health (2008, updated 2014). Diabetes and dietary supplements: In depth. National Center for Complementary and Integrative Health. https://nccih.nih.gov/health/diabetes/supplements.
Other Works Consulted
- American Diabetes Association (2017). Standards of medical care in diabetes—2017. Diabetes Care, 40(Suppl 1): S1–S135.
- Alemzadeh R, Ali O (2011). Diabetes mellitus. In RM Kliegman et al., eds., Nelson Textbook of Pediatrics, 19th ed., pp. 1968–1997. Philadelphia: Saunders.
- American Academy of Pediatrics (2013). Clinical Practice Guideline: Management of newly diagnosed type 2 diabetes mellitus (T2DM) in children and adolescents. Pediatrics, 131(2): 364–382. Also available online: http://pediatrics.aappublications.org/content/131/2/364.full.html.
- American Diabetes Association (2000). Type 2 diabetes in children and adolescents. Diabetes Care, 23(3): 381–389.
- American Diabetes Association (2012). Diabetes management at camps for children with diabetes. Diabetes Care, 35(Suppl 1): S72–S75.
- Jackson CC, et al. (2015). Diabetes care in the school setting: A position statement of the American Diabetes Association. Diabetes Care, 38(1): 1958–1963. DOI: 10.2337/dc15-1418. Accessed January 11, 2016.
- Li C (2009). Prevalence of pre-diabetes and its association with clustering of cardiometabolic risk factors and hyperinsulinemia among U.S. adolescents. Diabetes Care, 32: 342–347.
- Rewers M, et al. (2014). Diabetes mellitus. In WW Hay et al., eds., Current Diagnosis and Treatment: Pediatrics, 22nd ed., pp. 1097–1105. New York: McGraw-Hill.
- Rosenbloom AL (2011). Diabetes mellitus. In CD Rudolph et al., eds., Rudolph’s Pediatrics, 22nd ed., pp. 2104–2125. New York: McGraw-Hill.
- Siminerio LM, et al. (2014). Care of young children with diabetes in the child care setting: A position statement of the American Diabetes Association. Diabetes Care, 37(10): 2834–2842. DOI: 10.2337/dc14-1676. Accessed October 9. 2014.
- U.S. Department of Health and Human Services (2008). 2008 Physical Activity Guidelines for Americans (ODPHP Publication No. U0036). Washington, DC: U.S. Government Printing Office. Available online: http://www.health.gov/paguidelines/guidelines/default.aspx.
Current as of: April 16, 2019
Author: Healthwise Staff
Medical Review:John Pope MD – Pediatrics & Kathleen Romito MD – Family Medicine & Adam Husney MD – Family Medicine & Stephen LaFranchi MD – Pediatrics, Pediatric Endocrinology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.