Type 2 Diabetes
Topic Overview
What is type 2 diabetes?
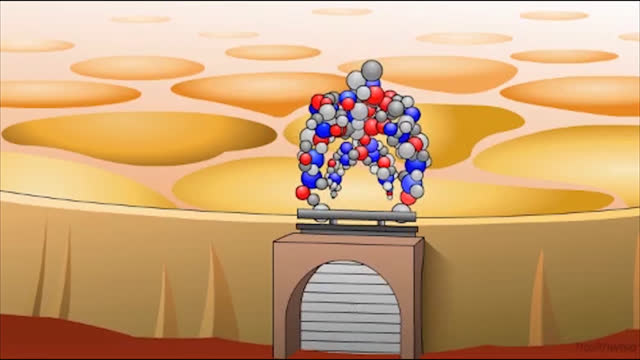
Type 2 diabetes happens when your body can’t use insulin the right way. Over time, the pancreas can’t make enough insulin.
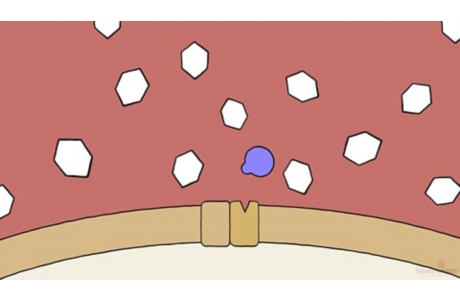
Insulin is a hormone that helps the body’s cells use sugar (glucose) for energy. It also helps the body store extra sugar in muscle, fat, and liver cells. Without insulin, this sugar can’t get into your cells to do its work. It stays in your blood instead. Your blood sugar level then gets too high.
High blood sugar can harm many parts of the body, such as the eyes, heart, blood vessels, nerves, and kidneys. It can also increase your risk for other health problems (complications).
Type 2 diabetes is different from type 1 diabetes. In type 1 diabetes, the body’s immune system destroys the cells that release insulin, so that over time the body can’t produce insulin at all. In type 2 diabetes, the body still makes some insulin, but it can’t use it the right way.
What causes type 2 diabetes?
You can get type 2 diabetes if:
- Your body doesn’t respond as it should to insulin. This makes it hard for your cells to get sugar from the blood for energy. This is called insulin resistance.
- Your pancreas doesn’t make enough insulin.
If you are overweight, get little or no exercise, or have type 2 diabetes in your family, you are more likely to have problems with the way insulin works in your body. Type 2 diabetes can be prevented or delayed with a healthy lifestyle, including staying at a healthy weight, making healthy food choices, and getting regular exercise.
What are the symptoms?
Some people don’t have symptoms, especially when diabetes is diagnosed early. This is because the blood sugar level may rise so slowly that a person may not know that anything is wrong.
The most common symptoms of high blood sugar include:
- Feeling very thirsty.
- Urinating more often than usual.
- Feeling very hungry.
- Having blurred vision.
You can get high blood sugar for many reasons, including not taking your diabetes medicines, eating more than usual (especially sweets), not exercising, or being sick or under a lot of stress.
If you’re taking diabetes medicine, you can also have problems with low blood sugar. These symptoms include:
- Sweating.
- Feeling weak.
- Feeling shaky.
- Feeling very hungry.
How is type 2 diabetes diagnosed?
If your doctor thinks that you have type 2 diabetes, he or she will ask you questions about your medical history, do a physical exam, and order a blood test that measures the amount of sugar in your blood.
How is it treated?
The key to treating type 2 diabetes is to keep blood sugar levels controlled and in your target range.
All of the following help to lower blood sugar:
- Making healthy food choices. Try to manage the amount of carbohydrates you eat by spreading them out over the day.
- Losing weight, if you are overweight
- Getting regular exercise
- Taking medicines, if you need them
It’s also important to:
- See your doctor. Regular checkups are important to monitor your health.
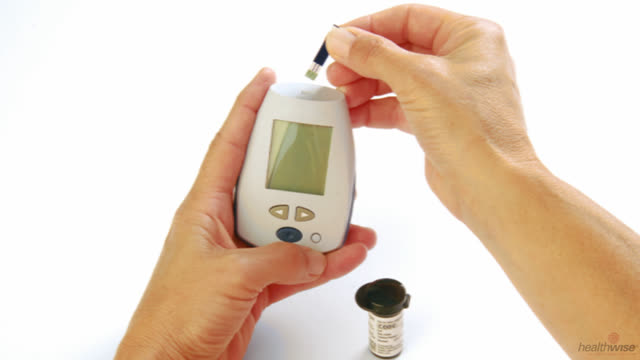
- Test your blood sugar levels. You have a better chance of keeping your blood sugar in your target range if you know what your levels are from day to day.
- Keep high blood pressure and high cholesterol under control. This can help you lower your risk of heart and large blood vessel disease.
- Quit smoking. This can help you reduce your risk of heart disease and stroke.
It seems like a lot to do—especially at first. You might start with one or two changes. Focus on checking your blood sugar regularly and being active more often. Work on other tasks as you can.
It can be hard to accept that you have diabetes. It’s normal to feel sad or angry. You may even feel grief. Talking about your feelings can help. Your doctor or other health professionals can help you cope.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
- Depression: Stop Negative Thoughts
- Diabetes: Checking Your Blood Sugar
- Diabetes: Coping With Your Feelings About Your Diet
- Diabetes: Counting Carbs if You Don’t Use Insulin
- Diabetes: Counting Carbs if You Use Insulin
- Diabetes: Dealing With Low Blood Sugar From Insulin
- Diabetes: Dealing With Low Blood Sugar From Medicines
- Diabetes: Giving Yourself an Insulin Shot
- Diabetes: Living With an Insulin Pump
- Diabetes: Preventing High Blood Sugar Emergencies
- Diabetes: Taking Care of Your Feet
- Diabetes: Using a Plate Format to Plan Meals
- Fitness: Adding More Activity to Your Life
- Fitness: Walking for Wellness
- High Blood Pressure: Checking Your Blood Pressure at Home
- Pregnancy and Diabetes: Planning for Pregnancy
Cause
Causes of diabetes
Type 2 diabetes occurs when your blood sugar (glucose) levels get too high because:
- Your body isn’t able to use insulin the right way. This makes it hard for your cells to get glucose from blood to make energy. This is called insulin resistance.
- Your pancreas doesn’t make enough insulin to make up for the insulin resistance. As type 2 diabetes gets worse, your pancreas may make less and less insulin. This is called insulin deficiency.
Your weight, how much physical activity you get, and your family history may affect the way your body responds to insulin.
Causes of high blood sugar
High blood sugar can happen if you:
- Skip a dose of your type 2 diabetes medicine or skip a required dose of insulin.
- Eat too much.
- Exercise less than what you are used to doing.
- Are taking medicines that raise blood sugar as a side effect, such as sleeping pills, some anti-inflammatory medicines (corticosteroids), and some decongestants.
- Are stressed or ill, especially if you aren’t eating or drinking enough. Plan ahead with your doctor and write down sick-day guidelines, which may include testing for ketones.
Being pregnant can also make your blood sugar levels go up.
If you take insulin, you may have some mornings when your blood sugar level is very high, even if it was low when you went to bed. This could be caused by the dawn phenomenon or the Somogyi effect. Talk with your doctor if this happens. You may need to check your blood sugar during the night to find out why your levels are high in the morning.
Causes of low blood sugar
You aren’t likely to get low blood sugar unless you take insulin or some kinds of oral medicines that can cause low blood sugar. You may get low blood sugar if you:
- Take too much diabetes medicine in a day, take your doses too close together, or take your full dose of medicine when you aren’t going to eat your usual amount of food.
- Exercise too much without eating enough food.
- Skip a meal.
- Drink too much alcohol, especially on an empty stomach.
- Take medicines for other conditions that can lower blood sugar, such as large doses of aspirin and medicines for mental health problems.
- Have problems with your kidneys.
- Start to have other problems with your glands and hormones, such as Addison’s disease or hypothyroidism.
Symptoms
Some people who have type 2 diabetes may not have any symptoms early on. Many people with the disease don’t even know they have it at first. But with time, diabetes starts to cause symptoms.
High blood sugar
Common symptoms of high blood sugar include:
- Being very thirsty.
- Urinating a lot.
- Losing weight without trying.
- Having blurry vision.
See more about symptoms of high blood sugar.
The higher your blood sugar rises, the more likely you are to have symptoms. If you have higher-than-normal blood sugar and don’t drink enough liquids, you can get dehydrated. This can make you feel dizzy and weak, and it can lead to an emergency called a hyperosmolar state.
To learn what to do in an emergency, see When to Call a Doctor.
Low blood sugar
When your blood sugar is too low, it can also cause problems. And it can happen suddenly. Quickly treating low blood sugar can help you avoid passing out (losing consciousness). You can pass out when your blood sugar gets very low. Low blood sugar can also lead to a heart attack.
Common symptoms of low blood sugar include:
- Sweating.
- Shakiness.
- Weakness.
- Hunger.
- Confusion.
See more about symptoms of low blood sugar.
If you aren’t able to tell when your blood sugar is too low (hypoglycemic unawareness), it’s a good idea to test your blood sugar often. But you’re not likely to get low blood sugar unless you take insulin or other diabetes medicines.
To learn what to do in an emergency, see When to Call a Doctor.
|
Know what your results mean  Rhonda O’Brien, certified diabetes educator As important as regular testing is, you also need to know what the results mean and how to use them. “Look for patterns. If your blood sugar is always high before lunch, take a look at what you had for breakfast. Maybe you need to make some changes.”— Rhonda |
What Happens
When you have type 2 diabetes, your body still makes insulin. But as time goes on, your pancreas may make less and less insulin, which will make it harder to keep your blood sugar in your target range. If your blood sugar gets too high and stays too high for too long, your risk for other health problems increases. Over time, high blood sugar can damage many parts of your body.
Eyes
High blood sugar levels may cause temporary blurred vision. Blurry vision, floaters, or flashes of light may be a sign of diabetic retinopathy, which can cause severe vision loss.
To learn more, see the topic Diabetic Retinopathy.
Feet and skin
You may have less feeling in your feet, which means that you can injure your feet and not know it. Blisters, ingrown toenails, small cuts, or other problems that may seem minor can quickly become more serious. If you develop serious infections or bone and joint deformities, you may need surgery (even amputation) to treat those problems. Common infections can quickly become more serious when you have diabetes.
Heart and blood vessels
High blood sugar damages the lining of blood vessels. This can lead to stroke, heart attack, or peripheral arterial disease. Erection problems can be an early warning sign of blood vessel disease and may mean a higher risk of heart disease.
Nerves
High blood sugar levels can damage nerves throughout your body. This damage is called diabetic neuropathy. There are three kinds of diabetic neuropathy:
- Diabetic peripheral neuropathy. This is damage to the nerves that sense pain, touch, hot, and cold. This type of nerve damage can lead to a deformity called Charcot foot. It can also lead to other problems that may require amputation.
- Autonomic neuropathy. This is damage to nerves that control things like your heartbeat, blood pressure, sweating, digestion, urination, and sexual function.
- Focal neuropathy. Most of the time, this affects just one nerve, usually in the wrist, thigh, or foot. It may also affect the nerves of your back and chest and those that control your eye muscles.
To learn more, see the topic Diabetic Neuropathy.
Kidneys
The kidneys have many tiny blood vessels that filter waste from your blood. High blood sugar can destroy these blood vessels. You won’t have any symptoms of kidney damage until the problem is severe. Then you may notice swelling in your feet or legs or all over your body.
To learn more, see the topic Diabetic Nephropathy.
Hearing
High blood sugar can damage the small blood vessels and nerves in the ear, causing hearing loss.
Teeth
Gum disease can make it harder to keep blood sugar in a target range. And high blood sugar can cause gum disease, loss of teeth, and healing problems in the mouth.
Mental health
Type 2 diabetes can raise your risk of depression. It may be caused by the stress of dealing with diabetes or by the effects that diabetes has on your body.
Being depressed can make it hard to eat healthy foods and to find the motivation to exercise. All of these things lead to higher blood sugar. By getting help for depression, you’ll feel better and may find it easier to stay motivated.
What Increases Your Risk
Risk factors you can’t changeinclude:
- Family history. If you have a parent, brother, or sister who has type 2 diabetes, you have a greater chance of developing the disease.
- Age. The risk for getting prediabetes and type 2 diabetes increases with age. And the number of children being diagnosed with type 2 diabetes is increasing. Usually, children who get type 2 diabetes have a family history of the disease, are overweight, and are physically inactive.
- Race and ethnicity. African Americans, Hispanics, Native Americans, Asian Americans, and Pacific Islanders are at higher risk than whites for type 2 diabetes.
- History of gestational diabetes. Women who have had gestational diabetes are at higher risk for developing type 2 diabetes later in life.
Risk factors you can change include:
- Being overweight. Staying at a healthy weight can lower your risk.
- Not getting enough exercise. Being active may help your body control blood sugar levels.
- Eating a diet that isn’t healthy. Making healthy food choices is important to avoid diabetes.
Other health problems can put you at risk for type 2 diabetes:
- Polycystic ovary syndrome (PCOS), a hormone imbalance that interferes with normal ovulation.
- A history of heart disease.
- High blood pressure.
- Your high-density lipoprotein (HDL) cholesterol is low and/or your triglyceride level is high.
- A skin condition called acanthosis nigricans, which is linked to insulin resistance.
- Prediabetes. Having prediabetes means that you are at risk for type 2 diabetes. It’s important to get treatment. If your fasting blood sugar levels are in the range from 100 mg/dL to 125 mg/dL, you are at increased risk for type 2 diabetes.footnote 1
If you’re worried
To see whether you are at risk for type 2 diabetes, see the website www.diabetes.org/are-you-at-risk/diabetes-risk-test. If you are at risk, you can discuss with your doctor how to make healthy changes in your life.
When to Call a Doctor
Call 911 or other emergency services right away if:
- You have symptoms of hyperosmolar state, such as:
- Blurred vision.
- Trouble staying awake or trouble being woken up.
- Fast, deep breathing.
- Breath that smells fruity.
- Belly pain, not feeling hungry, and vomiting.
- Feeling confused.
- Less common in type 2 diabetes is diabetic ketoacidosis (DKA), which has symptoms similar to those of hyperosmolar state. But DKA is still possible and very dangerous.
- You passed out (lost consciousness), or if you suddenly become very sleepy or confused. (You may have very low blood sugar, called hypoglycemia.)
Call a doctor if:
- You are sick and cannot control your blood sugar.
- You have been vomiting or have had diarrhea for more than 6 hours.
- You have a blood sugar level that stays higher than the level the doctor has set for you, for example, 300 mg/dL for two or more readings.
- You have blood sugar that stays lower than the level the doctor has set for you, for example, 70 mg/dL for two or more readings.
- You have symptoms of low blood sugar, such as:
- Sweating.
- Feeling nervous, shaky, and weak.
- Extreme hunger and slight nausea.
- Dizziness and headache.
- Blurred vision.
- Confusion.
Check with your doctor if:
- You often have problems with high or low blood sugar levels.
- You have trouble knowing when your blood sugar is low (hypoglycemia unawareness).
- You have questions or want to know more about diabetes.
Who to see
Health professionals who may be involved in your diabetes care include:
- A family doctor.
- A certified diabetes educator (CDE).
- A registered dietitian. All people newly diagnosed with diabetes should see a dietitian for help in choosing healthy foods.
- An endocrinologist.
If you have signs of complications of diabetes, such as nerve problems or kidney problems, you may be referred to a specialist. Learn more about the roles of the health professionals on a diabetes care team.
Exams and Tests
Diagnostic tests
If your doctor thinks that you may have diabetes, he or she will order blood tests to measure how much sugar is in your blood. The tests used are blood glucose tests and hemoglobin A1c.
To make a diagnosis of type 2 diabetes, your doctor will use your blood test results and the American Diabetes Association (ADA) criteria. He or she will also ask you questions about your medical history and do a physical exam for type 2 diabetes.
If it is hard to tell if you have type 2 or type 1 diabetes, your doctor may do a C-peptide test or test for autoantibodies. (Autoantibodies are produced when the body’s immune system does not work right.) These tests can help diagnose type 1 diabetes.
There are several types of autoantibodies, and some people may have them even before they show symptoms of type 1 diabetes. For people with a parent or sibling with type 1 diabetes, testing for autoantibodies and a higher-than-normal blood sugar level may be done to screen for an early stage of type 1 diabetes.
Some rare forms of diabetes (not type 1 or type 2 diabetes) are caused by a genetic problem and may need genetic testing to diagnose them.
Tests to monitor your health
You’ll need to see your doctor every 3 to 6 months. At each visit you’ll:
- Check your blood sugar levels since your last visit and review your target range.
- Check your blood pressure and start or adjust treatment if your blood pressure is high. Nerve and blood vessel damage can result from high blood pressure, leading to heart problems and strokes. For more information, see the topic High Blood Pressure.
- Have a hemoglobin A1c test. This blood test shows how steady your blood sugar levels have been over time.
Your doctor might suggest a cholesterol and triglyceride test based on your age or your risk for heart disease. Talk to your doctor about when a cholesterol test is right for you.
For more information, see When to Have a Cholesterol Test.
See a list of tests to monitor diabetes to help you remember what to do and when.
Review your progress regularly
Regular visits and checkups with your doctor are also a good time to:
- Review your meal plan.
- Review your physical activity.
- Review your mental health.
- Review your blood sugar records.
- Review your medicines.
These visits are also a good time to talk with your doctor about how you’re feeling. It’s normal to feel frustrated or overwhelmed with all there is to do. If you’re having trouble coping, your doctor can help. And if your health is changing and you have complications from diabetes, work with your doctor to make the right medical decisions for you. With your health and quality of life in mind, problem-solve and plan with your doctor.
Tests to do every year
- A complete eye exam by an ophthalmologist or optometrist. High blood sugar levels from diabetes can damage your eyes. This test can find problems early, such as diabetic retinopathy. If you do not have any signs of diabetic retinopathy, your doctor may recommend less frequent exams, for example, every 2 years.
- A foot exam for signs of problems. Nerve damage in your feet makes it hard to feel an injury or infection. Take off your socks each time you see the doctor to be sure you both remember to check your feet.
- A urine test, to check for protein. If protein is found, you’ll have more tests to help guide the best treatment. Protein in the urine can be a sign of kidney damage (diabetic nephropathy).
- A blood test for creatinine and glomerular filtration rate (GFR). This test is used to screen for kidney disease.
- A liver test. This test looks for damage to the liver.
- A thyroid-stimulating hormone test. Women over 50 years old or anyone with high cholesterol should have this test.
Dental checkups
- Dental exam. See your dentist twice a year for professional cleaning of your teeth and to look for gum disease. Seeing your dentist is one part of taking care of your teeth and gums when you have diabetes.
Eye exams during pregnancy
If you get pregnant, you will need to have an eye exam sometime during the first 3 months. You’ll also need close follow-up during your pregnancy and for 1 year after you have your baby. Pregnancy increases your risk for diabetic retinopathy. If you already have eye disease and get pregnant, the disease can quickly get worse.
Treatment Overview
Your treatment for type 2 diabetes will change over time to meet your needs. But the focus of your treatment will always be to keep your blood sugar levels within your target range. That will help prevent complications from type 2 diabetes, such as eye, kidney, heart, blood vessel, and nerve disease.
The keys to managing your type 2 diabetes are to:
- Make healthy food choices and be active. To learn more, see Living With Type 2 Diabetes.
- See your doctor regularly. To help you stay on track with your treatment, you’ll need regular tests. For more information, see Exams and Tests.
- Test your blood sugar. It’s important to track your blood sugar levels so you know if you are in your target range. For more information, see Living With Type 2 Diabetes.
- Take medicines, if you need them. For more information, see Medications.
- If you smoke, quit. Quitting can help you reduce your risk of heart disease and stroke. For help, see the topic Quitting Smoking.
- Keep high blood pressure and high cholesterol under control. Losing weight and getting plenty of exercise, such as walking at least 2½ hours a week, can help lower blood pressure. But you may also need to take medicines, such as an ACE inhibitor or beta-blocker, to achieve your goal. You may also need to take cholesterol-lowering medicines called statins.
Making big changes like quitting smoking or changing the way you eat is hard. But you can do it if you set small goals and celebrate your successes. For help, see the topic Change a Habit by Setting Goals.
Pregnancy and breastfeeding
Your treatment may change if you get pregnant. For example, some medicines could harm your baby. If your blood sugar gets too high while you’re pregnant, your baby might have problems at birth. Talk with your doctor.
And you can successfully breastfeed your baby when you have type 2 diabetes.
 One Woman’s Story: Gloria, 70 “Exercise really changed everything for me. The way I feel, my blood sugar, everything. It really works. I never felt better, stronger, healthier, or happier in my life.”— Gloria |
Prevention
Many people have prediabetes before they have type 2 diabetes. If you’re concerned about your risk, talk with your doctor. He or she will order tests to check your blood sugar levels. If you have prediabetes, you should be tested for type 2 diabetes every year. To learn more, see the topic Prediabetes.
You can take steps to prevent type 2 diabetes. Even small changes can make a difference, and it is never too late to start making healthier choices.
Stay at a healthy weight
A healthy weight is one that is right for your body type and height and is based on your body mass index (BMI) and the size of your waist (waist circumference). Losing just 7% of your body weight can help reduce your risk for type 2 diabetes. If you are age 20 or older, use the Interactive Tool: Is Your BMI Increasing Your Health Risks? to check your BMI. To use the tool, you’ll need to know your height, weight, and waist circumference.
Exercise regularly
Do activities that raise your heart rate. Try to do moderate activity at least 2½ hours a week. Or try to do vigorous activity at least 1¼ hours a week. It’s fine to be active in blocks of 10 minutes or more throughout your day and week.footnote 2
If your doctor says it’s okay, then try to do muscle-strengthening exercises at least 2 times a week. These exercises include push-ups and weight training. You can also use rubber tubing or stretch bands. You stretch or pull the tubing or band to build muscle strength. Be sure to work the major muscle groups: legs, hips, back, abdomen, chest, shoulders, and arms.
Walking groups or programs are great ways to start exercising and to stay motivated.
Using an exercise planning form( What is a PDF document? ) may help you and your doctor create a personalized exercise program.
Eat healthy foods
Review the dietary guidelines for good health, which are good for everyone, including people who have prediabetes or type 2 diabetes.
- Eat a balanced diet, including whole grains, lean sources of protein, and vegetables. Lose weight if you need to, by eating fewer calories and exercising more.
- Get enough fiber.
Take medicine if you need it
If exercise, eating healthy foods, and being at a healthy weight don’t help lower your blood sugar, you may need to take medicine. For people who have prediabetes, the medicine metformin can help prevent type 2 diabetes.
Living With Type 2 Diabetes
Making healthy choices
Making healthy choices is a big part of managing type 2 diabetes. The more you learn about the disease, the more motivated you may be to make good choices and follow your treatment plan.
Eat healthy foods
Eat a balanced diet, and try to manage the amount of carbohydrates you eat by spreading them out over the day.
The dietary guidelines for good health can help everyone form healthy eating habits, including people who have type 2 diabetes. It is especially important for people with type 2 diabetes to:
- Shift from eating unhealthy saturated fats to eating healthier unsaturated fats.
- Avoid foods that contain trans fat.
- Eat less salt.
- Be careful with alcohol, which affects your blood sugar. It can make problems from nerve damage, blood pressure, cholesterol, and weight even worse. Adult women should limit alcohol to 1 drink a day with a meal. Adult men should limit alcohol to 2 drinks a day with a meal. And women who are pregnant should not drink at all.
Be active
You don’t have to join a gym to get fit or be active. There are many things you can do, such as walking or even vacuuming.
Test your blood sugar
Work with your doctor to set your own target blood sugar range.
A continuous glucose monitor, or CGM, checks and records blood sugar day and night. Most CGMs sound an alarm if blood sugar levels are moving out of target range.
Having a record of your blood sugar over time can help you and your doctor know how well your treatment is working and whether you need to make any changes.
Take medicines, if you need them
Insulin and some diabetes medicines may cause low blood sugar.
Check your feet and skin daily
Check your feet and skin every day for signs of problems. Nerve damage makes it hard to feel an injury or infection.
Living and coping
Trying to manage your type 2 diabetes isn’t easy. Some days you may feel like it’s just too much work to do everything you need to do. There will be times when you just don’t feel like testing and tracking your blood sugar.
It’s normal to feel sad or even angry sometimes when you have a health problem. Even though you’ve had a while to get used to the idea of having type 2 diabetes, you may still have trouble adjusting. You may find it hard to stay motivated.
When you feel sad, give yourself time to adjust to your losses. If you feel overwhelmed, just try to focus on one day at a time. Do the best you can. You don’t have to be perfect.
Get the support you need
If you’re having trouble coping with your feelings, try talking with a counselor. A professional may make it easier to say things you wouldn’t talk about with friends or family.
If you have symptoms of depression, such as a lack of interest in things you used to enjoy, a lack of energy, or trouble sleeping, talk with your doctor. For more help, see the topic Depression.
You might also want to:
- Talk with friends and family about how you feel and any help you need.
- Ask a friend or family member to come to counseling with you.
- Talk to your spiritual adviser if you belong to a church or spiritual group. He or she will have experience helping people deal with their feelings.
- Join a support group. You can find one through your doctor, your local hospital, or the American Diabetes Association.
 One Man’s Story: Andy, 52 As a grocery manager, Andy is on his feet all day. He also likes to bowl and play basketball with his buddies. He started thinking about what he would do if he couldn’t walk, work, or play. “It finally just hit me how serious this disease is. I couldn’t keep ignoring it.”— Andy |
Taking care of yourself in other ways
Be aware of other things you can do to help yourself stay healthy.
- Wear medical identification at all times. You can buy medical identification such as bracelets, necklaces, or other kinds of jewelry at your local drugstore.
- Be careful when you are driving. For example, wear a medical ID bracelet and have quick-sugar foods with you.
- Be prepared so that you can prevent problems while you are traveling. You can do things to be prepared, such as taking extra medical supplies with you.
- Get a flu vaccine every year. When you have the flu, it can be harder to manage your blood sugar. It’s a good idea to get a pneumococcal vaccine for pneumonia and a vaccine for hepatitis B.
- Use vision aids if you have trouble with your eyesight.
Medications
How medicine helps manage diabetes
Some people with type 2 diabetes need medicines to help their bodies make insulin, decrease insulin resistance, or slow down how quickly their bodies absorb carbohydrates.
You may take no medicine, one medicine, or a few medicines. Some people need to take medicine for a short time, while others always need to take medicine. How much medicine you need depends on how well you can keep your blood sugar within your target range. You may need more medicine over time, even if you have good control of your blood sugar.
Medicines can help you manage your type 2 diabetes and other health problems, but only if you take them correctly. It can be hard to keep track of when and how to take your medicine, especially if you are taking more than one. Maybe you aren’t sure why you are taking a medicine or if it is working. Or you might have trouble paying for your medicine. For help, see the topic Quick Tips: Taking Medicines Wisely.
Medicine choices
- Medicines that you take by mouth. These include canagliflozin, glipizide, linagliptin, metformin, and pioglitazone.
- Medicines that are a shot. If you are having trouble controlling your blood sugar with pills, your doctor may suggest other medicines, including:
- Insulin. Insulin lets sugar (glucose) in the blood enter cells, where it is used for energy. Without insulin, the blood sugar level gets too high. Most of the time, people who take insulin use a combination of short-acting and long-acting insulin. This helps keep blood sugar within the target range. You may want to learn more about when insulin is needed for type 2 diabetes.
- Other shots, such as dulaglutide, exenatide, or liraglutide.
- Medicines to help prevent or treat complications. These include:
- Statins, such as atorvastatin (Lipitor), rosuvastatin (Crestor), or simvastatin (Zocor) to help prevent heart attack or stroke.
- Aspirin to help certain people lower their risk of a heart attack or stroke. But taking aspirin isn’t right for everyone, because it can cause serious bleeding. Talk to your doctor before you start taking aspirin every day.
- Angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) to help prevent or treat diabetic nephropathy.
- Phosphodiesterase-5 inhibitors (PDE-5 inhibitors), such as sildenafil (Viagra), vardenafil (Levitra), or tadalafil (Cialis), if you have erection problems. Check with your doctor before taking any of these medicines.
- Fibrates, such as fenofibrate (Tricor) or gemfibrozil (Lopid), to help lower triglycerides and increase HDL levels.
- Medicines for digestive problems. The type of medicine will depend on the problem you are having. For example, if you have gastroparesis, you may take metoclopramide (Reglan) or erythromycin.
- Nonprescription pain relievers, creams, or prescription oral or injection medicines if you have pain from peripheral neuropathy.
- Monitoring Your Medicines
Surgery
Weight-loss surgery
Experts recommend weight-loss surgery for people who have type 2 diabetes if their:footnote 3
- Body mass index (BMI) is 40 or more. For people in this group, surgery is recommended even when blood sugar is controlled with medicine or healthy habits.
- BMI is 35 or more. For people in this group, surgery is recommended when blood sugar is not controlled with medicine or healthy habits.
- BMI is 30 or more. For people in this group, some doctors may suggest surgery if blood sugar is not controlled with medicine or healthy habits.
If you are Asian, your doctor may recommend surgery with a lower BMI. Studies have shown that the risks from being overweight start at a lower BMI in people of Asian background.
Surgery for diabetes complications
Some complications from type 2 diabetes may need surgical treatment. For example:
- Surgery to remove the vitreous gel (vitrectomy) may be needed for diabetic retinopathy.
- Foot problems caused by diabetic neuropathy may lead to a need for amputation.
- Cardiovascular problems may require heart surgery.
Other Treatment
Avoid products that promise a “cure” for type 2 diabetes. For example, antioxidant supplements (vitamins E, C, and carotene) don’t cure type 2 diabetes. The American Diabetes Association does not recommend taking them.footnote 1
If you hear about something new to help type 2 diabetes, do some research to find out if it really works. You can also check with your doctor or a diabetes educator. Your health plan may also provide health information on its website.
These sources present information that is based on the analysis of a large body of medical evidence:
- Agency for Healthcare Research and Quality (AHRQ)
- Centers for Disease Control and Prevention (CDC)
- American Diabetes Association
Complementary therapies
Some complementary therapies may help relieve stress and muscle tension. They might help you feel better in general. But they shouldn’t be used as your only treatment for type 2 diabetes.
Talk with your doctor if you are using any of these treatments:
- Acupuncture
- Biofeedback
- Chiropractic therapy
- Herbal medicines and natural substances, such as antioxidants, vanadium, magnesium, or chromium
- Massage therapy
References
Citations
- American Diabetes Association (2019). Standards of medical care in diabetes—2019. Diabetes Care, 42(Suppl 1): S1–S193. Accessed December 17, 2018.
- U.S. Department of Health and Human Services (2008). 2008 Physical Activity Guidelines for Americans (ODPHP Publication No. U0036). Washington, DC: U.S. Government Printing Office. Available online: http://www.health.gov/paguidelines/guidelines/default.aspx.
- Rubino F, et al. (2016). Metabolic surgery in the treatment algorithm for type 2 diabetes: A joint statement by international diabetes organizations. Diabetes Care, 39(6): 861–877. DOI: 10.2337/dc16-0236. Accessed June 30, 2016.
Other Works Consulted
- American Diabetes Association (2013). Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care, 36(11): 3821–3842. DOI: 10.2337/dc13-2042. Accessed December 5, 2013.
- Bax J, et al. (2007). Screening for coronary artery disease in patients with diabetes. Diabetes Care, 30(10): 2729–2736. Also available online: http://care.diabetesjournals.org/content/30/10/2729.full?sid=7fd5fe8d-71f5-49c8-8e5e-98669526543e.
- Bolen S, et al. (2016). Diabetes medications for adults with type 2 diabetes: An update. Comparative Effectiveness Reviews, No. 173. (AHRQ Publication No. 16-EHC013-EF). Rockville (MD): Agency for Healthcare Research and Quality. http://www.ncbi.nlm.nih.gov/books/NBK362863. Accessed August 8, 2016.
- Brownlee M, et al. (2011). Complications of diabetes mellitus. In S Melmed et al., eds., Williams Textbook of Endocrinology, 12th ed., pp. 1462–1551. Philadelphia: Saunders.
- Centers for Disease Control and Prevention (2014). National diabetes statistics report: Estimates of diabetes and its burden in the United States, 2014. Centers for Disease Control and Prevention. http://www.cdc.gov/diabetes/pubs/statsreport14.htm. Accessed July 10, 2014.
- De Ferranti SD, et al. (2014). Type 1 diabetes mellitus and cardiovascular disease: A scientific statement from the American Heart Association and American Diabetes Association. Diabetes Care, published online August 11, 2014. DOI: 10.2337/dc14-1720. Accessed September 4, 2014.
- Fox CS, et al. (2015). Update on prevention of cardiovascular disease in adults with type 2 diabetes mellitus in light of recent evidence: A scientific statement from the American Heart Association and the American Diabetes Association. Diabetes Care, 38(9):1777–1803. DOI: 10.2337/dci15-0012. Accessed September 29, 2015.
- Giovannucci E, et al. (2010). Diabetes and cancer: A consensus report. Diabetes Care, 33(7): 1674–1685. Also available online: http://care.diabetesjournals.org/content/33/7/1674.full?sid=ccc0c9ea-6728-4ebc-ae85-d2eaa4f2a6ee.
- Handelsman Y, et al. (2015). American Association of Clinical Endocrinologists and American College of Endocrinology—Clinical practice guidelines for developing a diabetes mellitus comprehensive care plan—2015. Endocrine Practice, 21(Suppl 2): 1–87. Available online: https://aace.com/files/dm-guidelines-ccp.pdf. Accessed April 23, 2015.
- Inzucchi SE, et al. (2015). Management of hyperglycemia in type 2 diabetes, 2015: A patient-centered approach: Update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care, 38(1): 140–149. DOI: 10.2337/dc14-2441. Accessed February 18, 2015.
- Kirkman M, et al. (2012). Diabetes in older adults. Diabetes Care, 35(12), 2650–2664. Available online: http://care.diabetesjournals.org/content/35/12/2650.full.
- Kitabchi AE, et al. (2009). Hyperglycemic crises in adult patients with diabetes. Diabetes Care, 32(7): 1335–1343.
- Nix S (2013). Diabetes mellitus. In Williams’ Basic Nutrition and Diet Therapy, 14th ed., pp. 400–425. St. Louis: Mosby.
- Pignone M, et al. (2010). Aspirin for primary prevention of cardiovascular events in people with diabetes: A position statement of the American Diabetes Association, a scientific statement of the American Heart Association, and an expert consensus document of the American College of Cardiology Foundation. Circulation, 121(24): 2694–2701.
- Rogers L, et al. (2011). The charcot foot in diabetes. Diabetes Care, 34(9): 2123–2129. Also available online: http://care.diabetesjournals.org/content/34/9/2123.full?sid=32c9be6e-36be-44f6-8592-94442221751d.
- Rubino F, et al. (2016). Metabolic surgery in the treatment algorithm for type 2 diabetes: A joint statement by international diabetes organizations. Diabetes Care, 39(6): 861–877. DOI: 10.2337/dc16-0236. Accessed June 30, 2016.
- Schellenberg ES, et al. (2013). Lifestyle interventions for patients with and at risk for type 2 diabetes: A systematic review and meta-analysis. Annals of Internal Medicine, 159(8): 543–551. DOI: 10.7326/0003-4819-159-8-201310150-00007. Accessed November 25, 2013.
- Skyler JS, et al. (2009). Intensive glycemic control and the prevention of cardiovascular events: Implications of the ACCORD, ADVANCE, and VA Diabetes Trials: A position statement of the American Diabetes Association and a scientific statement of the American College of Cardiology Foundation and the American Heart Association. Diabetes Care, 32(1), 187–192.
- U.S. Department of Health and Human Services (2008). 2008 Physical Activity Guidelines for Americans (ODPHP Publication No. U0036). Washington, DC: U.S. Government Printing Office. Available online: http://www.health.gov/paguidelines/guidelines/default.aspx.
Current as of: April 16, 2019
Author: Healthwise Staff
Medical Review:E. Gregory Thompson MD – Internal Medicine & Kathleen Romito MD – Family Medicine & Martin J. Gabica MD – Family Medicine & Adam Husney MD – Family Medicine & David C.W. Lau MD, PhD, FRCPC – Endocrinology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.