Diabetic Neuropathy
Topic Overview
What is diabetic neuropathy?
Neuropathy means nerve disease or damage. Diabetic neuropathy is nerve damage caused by diabetes. People who have diabetes often have high blood sugar levels. Over time, high blood sugar levels can damage nerves throughout your body.
There are three kinds of diabetic neuropathy.
- Peripheral neuropathy is damage to peripheral nerves. These are the nerves that sense pain, touch, hot, and cold. They also affect movement and muscle strength. The nerves in the feet and lower legs are most often affected. This type of nerve damage can lead to serious foot problems. The damage usually gets worse slowly, over months or years.
- Autonomic neuropathy is damage to autonomic nerves. These nerves control things like your heartbeat, blood pressure, sweating, digestion, urination, and sexual function.
- Focal neuropathy affects just one nerve, usually in the wrist, thigh, or foot. It may also affect the nerves of your back and chest and those that control your eye muscles. This type of nerve damage usually happens suddenly.
What causes diabetic neuropathy?
Over time, high blood sugar levels from diabetes can damage nerves throughout your body. The higher your blood sugar levels, the more likely you are to have nerve damage. So controlling your blood sugar throughout your life is very important.
The older you get, and the longer you have diabetes, the more likely you are to have nerve damage. People who have diabetes who drink too much alcohol are also more likely to have nerve damage.
What are the symptoms?
Your symptoms will depend on which nerves are injured. You may not be able to feel pain, especially in your feet. This can lead to serious infections, because sores or other problems may not get treated.
When other parts of your body are affected, symptoms may include:
- Problems with digestion, such as bloating, belching, constipation, nausea and vomiting, diarrhea, and belly pain.
- Problems with body temperature, such as heavy sweating at night or when you eat certain foods. Some people may have reduced sweating, especially in their feet and legs.
- Problems with urination, such as finding it hard to tell when your bladder is full or finding it hard to empty your bladder completely.
- Sexual problems, such as erection problems in men and vaginal dryness in women.
- Heart and blood vessel problems, leading to poor circulation or low blood pressure. This may cause dizziness, weakness, or fainting when you stand or sit up from a reclining position.
- Trouble sensing when your blood sugar is low.
How is diabetic neuropathy diagnosed?
Your doctor will check how well you feel light touch and temperature and will test your strength and your reflexes. Tests such as electromyogram and nerve conduction studies may be done to confirm the diagnosis. You may need other tests to see which type of neuropathy you have and to help guide your treatment.
Doctors can’t test for all types of nerve damage. So it’s important to tell your doctor about any pain or weakness you feel. Also mention heavy sweating or dizziness and any changes in digestion, urination, and sexual function.
How is it treated?
Treatment involves keeping blood sugar levels in your target range. This will not cure the nerve damage, but it can help keep the damage from getting worse, and the pain might get better.
Other treatment depends on your symptoms:
- Pain may be treated with medicines.
- Digestive system problems or blood vessel problems may be treated with medicines.
- Blood pressure problems may be treated with medicines and by wearing support stockings (also called compression stockings).
- Sexual problems may be helped with medicines or devices to improve erections or with lubricating creams that help vaginal dryness.
- A splint or brace may be used for a pinched nerve.
When you have diabetes, you could have a sore or other foot problem without noticing it. Check your feet every day. An untreated problem on your foot can lead to a serious infection or even amputation.
Be clear with your doctor about what is helping you feel better and what is not. You and your doctor can work together to find the treatment that helps you the most.
Can diabetic neuropathy be prevented?
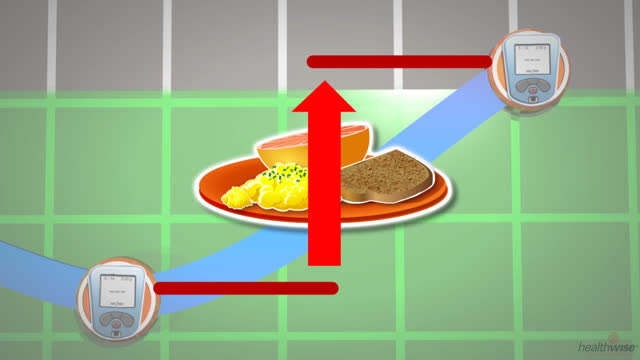
Keeping your blood sugar levels in your target range, set with your doctor, may help prevent neuropathy from ever developing. The best way to do this is by checking your blood sugar and adjusting your treatment. It is also important to get to and stay at a healthy weight by exercising and eating healthy foods.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Symptoms
Diabetic neuropathy—especially peripheral neuropathy—initially may not cause any noticeable symptoms. If you have diabetes, it is important to have regular medical checkups to check for signs of neuropathy and treat problems before they become serious.
Symptoms of diabetic neuropathy may vary depending on the type of neuropathy you have.
Symptoms of peripheral neuropathy
Peripheral neuropathy tends to develop slowly over months or years. In general, symptoms may include:
- Reduced feeling or numbness in the feet.
- Over time, tightness, burning, shooting, or stabbing pain in the feet, hands, or other parts of the body. Bone and joint deformities can develop, especially in the feet (such as Charcot foot).
- Greatly reduced or greatly increased sensitivity to light touch or temperature.
- Weakness and loss of balance and coordination.
Symptoms of autonomic neuropathy
Autonomic neuropathy may affect digestion, the body’s ability to regulate temperature, urination, sexual function, and heart and blood vessel function, including blood pressure. Symptoms may get worse during pregnancy. In general, symptoms may include:
- Frequent bloating, belching, constipation, heartburn, nausea and vomiting, diarrhea, and abdominal pain. These symptoms may point to gastroparesis, a condition that causes the stomach to empty much slower than normal.
- Extreme sweating of the torso, face, or neck at night or while eating certain foods, such as spicy foods and cheese. Some people may have reduced sweating, especially in their feet and legs.
- Trouble sensing when the bladder is full or problems emptying the bladder completely.
- Sexual problems, such as erection problems in men and vaginal dryness in women.
- Dizziness, weakness, or fainting when you stand or sit up from a reclining position (orthostatic hypotension).
- Trouble knowing when your blood sugar is low (hypoglycemia unawareness).
Symptoms of focal neuropathy
Symptoms of focal neuropathy usually appear suddenly. They may include:
- Pain, weakness, and motor problems in a single area of the body, such as a wrist, thigh, or foot. In cases of a compressed or pinched nerve, soreness and pain may develop more gradually over several weeks or months.
- Pain in and around one of your eyes, trouble moving an eye, and double vision. Focal neuropathy may sometimes affect the nerves that control your eye muscles.
Symptoms of focal neuropathy usually get better over time. But focal neuropathy may be permanent.
Exams and Tests
A diagnosis of diabetic neuropathy is based largely on your symptoms, medical history and physical examination. During a physical exam, your doctor may check how well you feel light touch, temperature, pain, vibration, and movement. Your doctor may also check your strength and reflexes. Electromyogram (EMG) and nerve conduction studies may be done to confirm a diagnosis. These tests measure how well and how quickly the nerves conduct electrical impulses. When nerve damage is present, the speed of nerve function slows.
Problems linked with autonomic neuropathy—which affects the nerves that control internal functions—can be hard to diagnose. When new symptoms develop, more testing may be needed to diagnose the problem, identify the cause, and guide treatment. For example, a study that measures how fast your stomach empties may be done if symptoms like bloating, indigestion, or vomiting suggest gastroparesis, a condition that causes the stomach to take too long to empty.
Nerve problems in people who have diabetes may be caused by other conditions, such as kidney disease, alcohol use disorder, or a vitamin B12 deficiency. A variety of laboratory tests (such as a complete blood count) may be used to screen for conditions other than diabetes that could be causing symptoms. Your symptoms and medical history will determine which tests are needed.
Early detection
For some diseases, doctors can use screening tests to look for problems before you have any symptoms. But doctors can’t test for all types of autonomic or focal neuropathy. So it is important to report to your doctor any pain, weakness, or motor problems you have. Also mention any changes in digestion, urination, sexual function, sweating, or dizziness. Your doctor will also look for signs of autonomic neuropathy during your physical exams.
The American Diabetes Association (ADA) recommends that people who have diabetes see a doctor to examine their feet for cracked or peeling skin, excessive or reduced sweating, blisters, calluses, ulcers, signs of infection, bone and joint abnormalities, and walking and balance—during each medical visit. The ADA also recommends a complete foot exam by a doctor at least once a year. This examination can detect a loss of sensation in your feet, which can lead to more serious foot problems.footnote 1
Treatment Overview
Good control of diabetes over time is the key to treating diabetic neuropathy. There is no cure for neuropathy, but keeping your blood sugar within a target range can reduce symptoms and prevent them from getting worse.
To help control your diabetes, eat food that is good for you and exercise. Controlling diabetes means maintaining blood sugar levels (A1c) within the target range. This will do more than anything else to help prevent diabetic neuropathy from getting worse.
Initial and ongoing treatment
Treatment for diabetic neuropathy depends on your symptoms and the type of neuropathy that you have. In general, treatment focuses on reducing current symptoms and preventing the condition from getting worse by keeping your blood sugar level within your target range. You can keep your blood sugar levels within the target range by taking your insulin or oral diabetes medicine as prescribed, checking your blood sugar levels, following your diet for diabetes, exercising, and seeing your doctor regularly.
Also, it is important to properly care for your feet when you have diabetic neuropathy. Diabetic neuropathy may cause a loss of feeling in your feet. It is possible for a sore or other foot problem to go unnoticed. Without proper foot care, an untreated foot sore can lead to a serious infection or possibly amputation.
It is also wise to maintain healthy habits such as seeing your doctor regularly, controlling your blood pressure, eating a balanced diet, exercising regularly, not smoking, and limiting or avoiding alcohol. Further treatment depends on the specific type of diabetic neuropathy that you have along with your current symptoms.
Peripheral neuropathy
Many people with peripheral neuropathy have mild to severe pain in specific parts of their bodies. Talk with your doctor about treatment that can reduce your pain and improve your physical functioning, mood, and mental well-being. Some people find these treatments helpful:
- Medicines such as pain relievers or creams to relieve pain. Prescription medicines often used to reduce pain from diabetic neuropathy may include medicines that are more commonly used to treat depression, such as tricyclic antidepressants and the antidepressant duloxetine hydrochloride, and medicines that control seizures, such as pregabalin and gabapentin. These medicines may be tried to reduce your pain even though you do not have depression or seizures.
- Complementary therapies such as acupuncture and biofeedback
- Physical therapysuch as exercises, stretching, and massage. If you are told to use heat or ice, be careful. Neuropathy can make it hard for you to feel changes in temperature.
- Transcutaneous electrical nerve stimulation (TENS), which is a type of therapy that reduces pain by applying brief pulses of electricity to nerve endings in the skin
Autonomic neuropathy
Autonomic neuropathy—which affects nerves that regulate internal functions—can affect digestion, urination, sweating, sexual function, blood pressure, and other involuntary body functions. Some symptoms of autonomic neuropathy can be hard to manage, but others respond well to treatment:
- Mild constipation.Eating small, frequent meals that are high in fiber and low in fat may help.
- Frequent diarrhea. Eating foods that are high in fiber may help. You may need medicines that slow the rate at which digested food and waste travel through the intestines, or you may need antibiotics such as amoxicillin, metronidazole, or tetracycline.
- Mild gastroparesis. This is a condition that causes the stomach to empty very slowly. It may get better if you eat small, frequent meals that are low in fiber and fat. Medicines that help the stomach empty more quickly may also be needed. Controlling blood sugar levels may reduce symptoms of gastroparesis.
- Abnormal sweating. If you sweat a lot, try to avoid intense heat and humidity. If you don’t sweat enough, you can use moisturizers to help with dry or cracked skin. Drinking more water can prevent overheating. Try to avoid places that are very hot or very cold.
- Lack of awareness of low blood sugar level. This is also called hypoglycemia unawareness. You can adjust your insulin and allow your blood sugar levels to be a little bit higher than the target range. Usually it is recommended that you keep your A1c in a target range.
- Urinary problems. Urinary problems can be treated with antibiotics for urinary tract infections and medicines to improve bladder control.
- Sexual problems. Your doctor may suggest using medicines or devices to improve erections. Or you may need nonprescription lubricants and estrogen creams for vaginal dryness.
- Blood pressure problems. High blood pressure may be treated with angiotensin-converting enzyme (ACE) inhibitors, such as benazepril and enalapril. Low blood pressure can be treated with medicines and by wearing support stockings (also called compression stockings).
Treatment if the condition gets worse
If diabetic neuropathy gets worse, you may have serious problems such as severe gastroparesis, bladder infections, or foot problems. In addition to keeping your blood sugars in your target range and taking good care of your feet, you may need further treatment if diabetic neuropathy progresses.
Diabetic neuropathy is a major risk factor for foot infections or foot ulcers leading to amputation. It is possible to have permanent disfigurement in one or both of your feet (such as Charcot foot) from diabetic neuropathy. Surgery is sometimes needed to correct deformed joints that can result from Charcot foot.
Severe gastroparesis may require other treatment, such as medicines that empty the stomach more quickly or a feeding tube that is inserted into the stomach.
Severe bladder infections or other bladder problems, such as loss of control, may require further diagnostic testing and treatments such as medicines or surgery to improve bladder function.
Also, it is common to experience symptoms of depression with any chronic disease, such as diabetes or diabetic neuropathy. Seeking help for depression may improve your overall well-being and aid in the treatment of your condition.
What to think about
No matter what you or your doctor try, you may not be pain-free. Be clear with your doctor about what is helping and what is not. You and your doctor can work together to find the right combination of medicine and other treatments to help you the most.
References
Citations
- American Diabetes Association (2019). Standards of medical care in diabetes—2019. Diabetes Care, 42(Suppl 1): S1–S193. Accessed December 17, 2018.
Other Works Consulted
- Brannagan TH (2010). Acquired neuropathies. In LP Rowland, TA Pedley, eds., Merritt’s Neurology, 12th ed., chap. 134, pp. 832–833. Philadelphia: Lippincott Williams and Wilkins.
- Brownlee M, et al. (2011). Complications of diabetes mellitus. In S Melmed et al., eds., Williams Textbook of Endocrinology, 12th ed., pp. 1462–1551. Philadelphia: Saunders.
- Freeman R (2010). Diabetic neuropathy. In RS Beaser, ed., Joslin’s Diabetes Deskbook: A Guide for Primary Care Providers, 2nd ed., pp. 499–522. Boston, MA: Joslin Diabetes Center.
- Hunt DL (2011). Diabetes: Foot ulcers and amputations, search date September 2010. Online version of BMJ Clinical Evidence: http://www.clinicalevidence.com.
- Masharani U, German MS (2011). Pancreatic hormones and diabetes mellitus. In DG Gardner, D Shoback, eds., Greenspan’s Basic and Clinical Endocrinology, 9th ed., pp. 573–655. New York: McGraw-Hill.
Current as of: April 16, 2019
Author: Healthwise Staff
Medical Review:E. Gregory Thompson MD – Internal Medicine & Kathleen Romito MD – Family Medicine & Adam Husney MD – Family Medicine & Karin M. Lindholm DO – Neurology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.