Drug-Eluting Stents
Topic Overview
Drug-eluting stents prevent a coronary artery from narrowing again after angioplasty. They are coated with medicine that prevents scar tissue from growing into the artery.
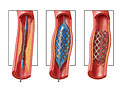
Stents are small, expandable tubes that are inserted during angioplasty into a narrowed or blocked section of the coronary artery to open the artery and improve blood flow.
See a picture of a stent. Drug-eluting stents are used more often than bare-metal stents.
How are stents placed in an artery?
During an angioplasty, a stent is inserted into the coronary artery.
View the slideshow on angioplasty to see how an angioplasty is done.
See a picture of stent placement.
During angioplasty, the balloon is placed inside the stent and inflated, which opens the stent and pushes it into place against the artery wall to keep the narrowed artery open. Because the stent is like woven mesh, the cells lining the blood vessel grow through and around the stent to help secure it. Your doctor may use a bare-metal stent or a drug-eluting stent.
To decide which type of stent to use, your doctor will consider your overall health and your risk of a heart attack. He or she will also consider whether you can and want to take blood-thinning medicines for at least 1 year.
How do drug-eluting stents work?
All stents have a risk that scar tissue will form and narrow the artery again. This scar tissue can block blood flow. But drug-eluting stents are coated with drugs that prevent scar tissue from growing into the artery. Drug-eluting stents may lower the chance that you will need a second procedure (angioplasty or surgery) to open the artery again.
Living with a stent
You don’t have to live differently if you have a stent. But you’ll want to take care of your heart by eating healthy, being active, and taking your medicines. There are a few precautions to follow.
Aspirin and other antiplatelet medicines. Take your blood-thinning medicines to prevent a heart attack or stroke. After angioplasty, you will probably take aspirin plus another antiplatelet. If you get a drug-eluting stent, you will probably take both of these medicines for at least 6 months. If you get a bare-metal stent, you may take both medicines for at least 1 month. If you had a heart attack, you may take both medicines for at least 1 year. If you have a high risk of bleeding, your doctor may shorten the time you take these medicines. You can work with your doctor to decide how long you will take both of these medicines. This decision may depend on your risk of a heart attack, your risk of bleeding, and your preferences about taking medicine.
Stent identification card. Carry your stent identification card. Your doctor will give you a card for your wallet or purse that you can show to your health professionals so they know that you have a stent.
References
Other Works Consulted
- Levine GN, et al. (2016). 2016 ACC/AHA Guideline focused update on duration of dual antiplatelet therapy in patient with coronary artery disease. Circulation, published online March 29, 2016. DOI: 10.1161/CIR.0000000000000404. Accessed March 29, 2016.
- Malenka DJ, et al. (2008). Outcomes following coronary stenting in the era of bare-metal vs the era of drug-eluting stents. JAMA, 299(24): 2868–2876.
- O’Gara PT, et al. (2013). 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: Executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation, 127(4): e362–e425.
Current as of: April 9, 2019
Author: Healthwise Staff
Medical Review:Rakesh K. Pai, MD – Cardiology, Electrophysiology & E. Gregory Thompson, MD – Internal Medicine & Martin J. Gabica, MD – Family Medicine & Adam Husney, MD – Family Medicine & Stephen Fort, MD, MRCP, FRCPC – Interventional Cardiology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.