Lupus (Systemic Lupus Erythematosus)
Topic Overview
What is systemic lupus erythematosus, or lupus?
Lupus is an autoimmune disease. This means that the body’s natural defense system (immune system) attacks healthy tissues instead of attacking only things like bacteria and viruses. This causes inflammation.
Although some people with lupus have only mild symptoms, the disease is lifelong and can become severe. But most people can control their symptoms and prevent severe damage to their organs. They do this by seeing their doctors often for checkups, getting enough rest and exercise, and taking medicines.
This topic focuses on systemic lupus erythematosus (SLE), the most common and most serious type of lupus. But there are other types of lupus, such as discoid or cutaneous lupus, drug-induced systemic lupus, and neonatal lupus.
What causes lupus?
The exact cause of lupus is not known. Experts believe that some people are born with certain genes that affect how the immune system works. These people are more likely to get lupus. Then a number of other things can trigger lupus attacks. These include viral infections, including the virus that causes mononucleosis, and sunlight.
Although these things can trigger lupus, they may affect one person but not another person.
What are the symptoms?
Lupus symptoms vary widely, and they come and go. The times when symptoms get worse are called relapses, or flares. The times when symptoms are under control are called remissions.
Common symptoms include feeling very tired and having joint pain or swelling (arthritis), a fever, and a skin rash. The rash often happens after you have been in the sun. You may have mouth sores and hair loss. Over time, some people with lupus have problems with the heart, lungs, kidneys, blood cells, or nervous system.
How is lupus diagnosed?
There is no single test for lupus. Because lupus affects different people in different ways, it can be hard to diagnose.
Your doctor will check for lupus by examining you, asking you questions about your symptoms and past health, and doing some urine and blood tests.
How is it treated?
Treatment for lupus may include:
- Corticosteroid cream for rashes.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) for mild joint or muscle pain and fever.
- Antimalarial medicines to treat fatigue, joint pain, and skin rashes.
- Corticosteroid pills if other medicines aren’t controlling your symptoms.
The doctor may also recommend other medicines that slow down the immune system (immunosuppressants).
How can you manage lupus?
One of the goals of controlling mild to moderate lupus symptoms is to prevent flares. You can:
- Rest to reduce stress.
- Avoid the sun. Wear sunscreen and protective clothing when you are outside.
- Exercise regularly to prevent fatigue and joint stiffness.
- Stop smoking.
- Watch your symptoms. If they seem to be getting worse, take steps to control them. For example, if your fatigue, pain, or rash gets worse, it may be a sign of a flare.
With good self-care, most people who have lupus can keep doing their regular daily activities.
It is important to learn about lupus so that you can understand how it might affect your life and how you can best cope with it. Also, help your family and friends understand your limitations and needs when your symptoms flare. Build a support system of family, friends, and health professionals.
Cause
The exact cause of lupus is not known. Experts believe that some people are born with certain genes that affect how the immune system works. These people are more likely to get lupus. Then a number of other things can trigger lupus attacks. These include certain medicines, certain chemicals, tobacco smoke, certain infections, and sunlight. Although these things can trigger lupus, they may affect one person but not another person.
Symptoms
Lupus symptoms depend on what body organs are affected and how seriously they are affected.
Common symptoms
Many people have these symptoms:
- Fatigue: Lupus causes mild to extreme fatigue. Even mild cases of lupus make it hard to do daily activities and exercise. Increased fatigue is a classic sign that a symptom flare is about to occur.
- Joint and muscle pain: Joints may be painful, red, and warm. They may swell. Morning stiffness may also be felt. Lupus arthritis often occurs on both sides of the body at the same time. It’s most often felt in the wrists, the small joints of the hands, and the elbows, knees, and ankles.
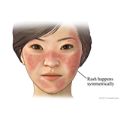
- Skin problems: Skin rashes are often an important clue to the diagnosis. Many people have a butterfly rash over the cheeks and bridge of the nose. Other common skin symptoms include skin sores or flaky red spots on the arms, hands, face, neck, or back; mouth or lip sores; and a scaly, red or purple raised rash on the face, neck, scalp, ears, arms, and chest.
- Sensitivity to light: Exposure to ultraviolet light (such as sunlight or tanning parlors) typically makes the skin rash worse and can trigger lupus flares. Many people with lupus are sensitive to light, with fair-skinned people tending to be more sensitive.
- Fever: People with lupus will sometimes have a low-grade fever related to the disease. Fever is sometimes a first sign of the disease.
- Changes in weight: People with lupus may lose weight when their disease is active (flaring).
- Swollen glands: Over time, people with lupus may get swollen lymph glands during a flare.
- Headaches: These are usually related to stress and tension but can be related to a lupus flare. Many people who have lupus get migraine headaches.
Other symptoms
- Raynaud’s phenomenon: Some people with lupus have Raynaud’s phenomenon. It affects the small vessels that supply blood to the skin and the soft tissues under the skin of the fingers and toes. It causes them to turn white and/or blue or red. The skin affected will feel numb, tingly, and cold to the touch.
- Hair loss: People with lupus may have periods of hair loss, either in patches or spread evenly over the head. This hair loss usually isn’t permanent.
- Inflammation of blood vessels in the skin (cutaneous vasculitis): Inflammation or bleeding from the blood vessels can lead to small or large blue spots or small reddish spots on the skin or nail beds.
- Symptoms from complications. Complications include nervous system, heart, and lung problems.
Other conditions with symptoms similar to lupus include fibromyalgia and myalgic encephalomyelitis/chronic fatigue syndrome.
What Happens
The course of lupus varies by individual and is hard to predict, because symptoms come and go. Lupus usually develops so slowly that a person may not notice the symptoms for a long time. Sometimes lupus develops and progresses rapidly.
Periods of time when you have lupus symptoms are called flares or relapses. Periods of time when your symptoms are under control are called remissions. Flares and remissions can occur abruptly, unexpectedly, and without clear cause. There is no way to predict when a flare will happen, how bad it will be, or how long it will last. When you have a lupus flare, you may have new symptoms in addition to those you have had in the past.
Children can get lupus, though it more commonly develops in the teen years or later. Lupus in children appears to be more severe than in adults when vital organs, such as the kidneys and heart, are involved.
Some people with lupus have complications such as kidney and heart problems. There are also concerns if you have lupus and are pregnant.
Living with lupus
Most people with lupus are able to continue their usual daily activities. But when your symptoms flare, you may find that you need to cut back on your activity level, get help with child care, or change the way you work. Or you may find that you need time off from all daily activities.
Most people with lupus can expect to live a normal or near-normal life span. This depends on how severe your disease is, whether it affects vital organs (such as the kidneys), and how severely these organs are affected.
A key to living with lupus is communication. Stay in touch with your doctor about new or increased symptoms, side effects of medicines, and your worries and anxieties. Talk with your family, friends, and employer so they understand what you can and can’t do, and what they can do to support you.
What Increases Your Risk
The chances of developing lupus are higher in people who:
- Are female.
- Are black.
- Are between the ages of 15 and 45.
- Have a family history of lupus.
- Take medicines that are associated with drug-induced systemic lupus.
Certain things can trigger lupus attacks. These may include:
- Exposure to ultraviolet light, usually from sunlight.
- Smoking. Smoking also may make getting lupus more likely, and make it more severe.
- Some medicines.
- Some infections. Some people who have cytomegalovirus (CMV), parvovirus (such as fifth disease), and hepatitis C infections eventually get lupus. The Epstein-Barr virus has been linked to lupus in children.
- Chemical exposure. Suspected chemical toxins include trichloroethylene in well water and silica dust. Hair dyes and straighteners, linked to lupus in the past, are no longer thought to trigger lupus.
What about hormones?
Hormones, including those used for hormone therapy or birth control, don’t cause lupus. But they may have some effect on it.
- Most women don’t have symptom flares during pregnancy, but a few women do when their estrogen levels are high.
- Although most women who get lupus are ages 15 to 45, when estrogen levels are higher, a number of women get lupus after menopause, when estrogen levels are low.
- The hormones in birth control pills have not proved to be harmful in women who have stable, moderate lupus.footnote 1 Women with lupus that isn’t well controlled may choose to use nonhormonal birth control methods. These include a copper intrauterine device (IUD), a condom, or a diaphragm. To learn more, see the topic Birth Control.
Talk with your doctor about whether you should use hormonal birth control or hormone therapy.
When should you call your doctor?
Call 911 or other emergency services immediately if you have symptoms of a heart attack. These may include:
- Chest pain or pressure, or a strange feeling in the chest.
- Sweating.
- Shortness of breath.
- Nausea or vomiting.
- Pain, pressure, or a strange feeling in the back, neck, jaw, or upper belly, or one or both shoulders or arms.
- Lightheadedness or sudden weakness.
- A fast or irregular heartbeat.
After you call 911, the operator may tell you to chew 1 adult-strength or 2 to 4 low-dose aspirin. Wait for an ambulance. Do not try to drive yourself.
Call 911 or other emergency services immediately if you have one or more of the following signs of a stroke:
- Sudden numbness, tingling, or weakness in or an inability to move (paralysis) part or all of one side of the body (such as the face, arm, and leg)
- Vision changes that come on suddenly, such as dimness, blurring, double vision, or loss of vision in one or both eyes
- A seizure
- Sudden difficulty speaking or understanding speech
- Sudden nausea or vomiting
- A sudden, severe headache, different from previous headaches, that occurs without a known cause
- Sudden dizziness, clumsiness, staggering, or fainting (loss of consciousness)
Call a doctor immediately if you:
- Are short of breath.
- Have blood in your urine or are urinating less often and in smaller amounts than usual.
- Have a fever over 100.5°F (38.1°C), with or without headache and body aches, but you haven’t recently been exposed to a cold or the flu.
- Experience depression or any changes in behavior or thinking.
- Have numbness or tingling in the hands or feet.
- Are dizzy or have muscle weakness.
- Have swelling of the lower legs or feet.
Call a doctor as soon as possible if you develop any new symptoms of lupus. Also call your doctor if any symptoms that you have had for a period of time get worse.
If you have not been diagnosed with lupus and you have symptoms such as joint pain, fatigue, or skin rashes, see your doctor or tell your doctor about your concerns at your next medical appointment.
Who to see
To evaluate initial symptoms and treat mild lupus, you can talk with:
- A family medicine doctor or an internist.
- A rheumatologist.
- An immunologist.
For long-term management of complicated lupus, talk with:
- A rheumatologist.
- An immunologist.
For more complicated cases of lupus, a rheumatologist is usually the primary doctor. Other specialists are consulted as needed.
- For mental health problems such as depression, anxiety, psychosis, or other behavioral changes, see your family medical doctor or internist, or a psychiatrist.
- For the treatment of organ problems, a doctor who specializes in diseases of that particular organ system may work together with a rheumatologist or immunologist. The following practitioners typically treat vital organ problems caused by lupus:
Exams and Tests
Lupus can be hard to recognize, and it sometimes takes weeks to years to diagnose. Lupus affects different people in different ways. And it can take time for symptoms to develop.
Your doctor will record your medical history and do a physical exam. He or she will check for certain criteria to help diagnose lupus. These criteria include the butterfly rash and joint swelling.
Diagnosis and disease monitoring
If you have symptoms of lupus and you have a positive antinuclear antibody (ANA) test result, further testing may not be needed.
If your doctor feels that further testing is needed, you may have one or more of the following tests:
- Other antibody blood tests
- Complement test
- Erythrocyte sedimentation rate (ESR, or sed rate) or C-reactive protein (CRP)
- Complete blood count (CBC)
- Urinalysis
- Lupus anticoagulant test, such as a partial thromboplastin time test
Checking for possible organ damage
As part of ongoing treatment for lupus, you may have a:
- Urinalysis to check for protein and cells, signs of possible kidney problems.
- Kidney biopsy, if your doctor sees signs of kidney inflammation. This test may help your doctor find the best treatment for you. Only a small number of people with lupus need a kidney biopsy.
To look for other possible causes of symptoms, imaging tests are sometimes done, depending on which organ systems are involved. Imaging tests include CT scan, echocardiogram, MRI, and X-rays.
Treatment Overview
Your treatment choices for lupus depend on how severe your symptoms are, whether your organs are affected, and how much your symptoms are affecting your daily life. Your treatment plans should be tailored to your individual needs and will change over time, as the disease flares or ebbs. There currently is no cure for lupus.
Treatment for mild lupus
The goal of treatment for mild lupus is to prevent symptom flares—when fatigue, joint pain, and rash get worse.
- Get regular checkups with your doctor, instead of waiting until your disease flares. When flares do occur, the goal is to treat them right away to limit any damage to body organs.
- Avoid the sun. If you must be in the sun, cover your arms and legs, wear a hat, and apply broad-spectrum sunscreen (covering both UVA and UVB rays) with a high sun protection factor (such as SPF 50) to protect your skin.
- Use corticosteroid cream for rashes.
- Take acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) for mild joint or muscle pain and fever. Be safe with medicines. Read and follow all instructions on the label.
- Get plenty of rest.
- Take antimalarial medicines, especially for skin rashes. They also help with fatigue and joint and muscle pain.
- Take low-dose corticosteroids if NSAIDs aren’t effective in controlling your symptoms.
Treatment for more severe lupus
If your lupus is causing or threatening organ damage, is life-threatening, or is seriously impacting your quality of life, you may also need to take:
- Corticosteroids in higher doses, either in pills or through a vein in your arm (IV).
- Medicine that suppresses your immune system (immunosuppressants).
To learn more, see Medications.
If you develop serious kidney disease that cannot be controlled with medicine, you may need dialysis or a kidney transplant.
Self-care
Good self-care is essential to managing lupus. A healthy lifestyle may reduce how often you have flares and how severe they are. It can improve your quality of life. Good self-care also helps decrease the risk of heart attack and stroke.
Self-care includes getting regular exercise and eating a healthy diet. To learn more, see Home Treatment.
What to think about
Taking corticosteroids by mouth and being physically inactive put people with lupus at great risk of bone thinning (osteoporosis). Getting an adequate supply of calcium and vitamin D may slow the bone thinning process. Your doctor may also prescribe bisphosphonates, a type of medicine that is also used for the prevention and treatment of osteoporosis. To learn more, see the topic Osteoporosis.
Lupus treatment is complicated by several things. The course and pattern of lupus symptoms vary widely. Flares and remissions can occur at any time, making it hard to tell how you are responding to treatment or which treatments are most helpful. Some treatment side effects can be as troubling as the symptoms of lupus.
It may not be possible to completely eliminate all of your symptoms for long periods of time, especially without the side effects from medicines. Work closely with your doctor to reach a balance between reasonably controlling your symptoms, preventing damage to your organs, and minimizing side effects of long-term drug treatment. For example, you may take a dose of medicine that will control lupus enough to prevent organ damage, but you may still have symptoms such as mild skin rash, muscle aches, and joint pain.
Using higher doses of medicines for a long time increases the risk of serious side effects. Your doctor will prescribe a dose that controls only the most serious, life-threatening symptoms and balances the risks of the medicines with the benefits of controlling your symptoms.
Prevention
There is currently no way to prevent lupus. But people who smoke may be more likely to get lupus. Avoiding smoking and perhaps other tobacco products may decrease your risk.
Home Treatment
Good self-care is essential to managing lupus. Learn to recognize your body’s warning signs of a flare. Warning signs may include increased fatigue, joint pain, rash, or fever. When you notice any of these signs, take steps to control your symptoms.
Dealing with stress and fatigue
Stress may trigger lupus symptoms. Keep your stress level as low as you can.
- Keep your daily schedule as simple as possible.
- Keep your list of obligations to others to a bare minimum.
- Delegate to others.
- Exercise regularly. A daily walk, for example, can reduce stress, clear your head, improve your mood, and help fight fatigue.
- Use relaxation techniques such as meditation, yoga, and guided imagery to calm your body and mind.
Fatigue is common in people with lupus. To fight fatigue:
- Get plenty of rest. Some people with lupus need up to 12 hours of sleep every night.
- Pace yourself. Limit tiring activities.
- Ask others for help. Don’t try to do everything yourself.
- Take short breaks from your usual daily activities. Consider cutting down on work hours or getting help with parenting responsibilities, at least during periods when lupus symptoms are severe.
- Exercise regularly. Physical activity boosts energy and helps you stay in good condition. Walking and swimming are good forms of exercise for people with lupus.
- If you suspect that depression is contributing to your fatigue, get prompt treatment from your doctor, a mental health professional, or both.
Taking care of your skin and health
Take care of your skin. Ask your doctor about the use of corticosteroid creams to relieve skin symptoms that are particularly troublesome. If you are bothered by the way a lupus rash looks on your face or if you have scars from lupus, you can try makeup, such as Covermark, to cover the rash or scars.
Ultraviolet (UVA and UVB) light triggers disease flares in most people who have lupus. Exposure to ultraviolet light, as from sunlight, can trigger or start skin rash, joint pain, or fatigue, or it can make these symptoms worse. To minimize your exposure to ultraviolet light:
- Avoid the sun. If you must be in the sun, cover your arms and legs, wear a hat, and apply broad-spectrum sunscreen (covering both UVA and UVB rays) with a high sun protection factor (50 SPF or higher) to protect your skin. Reapply sunscreen after swimming, sweating, or toweling off. Experiment with sunscreens. Some may irritate your skin or wash off too easily.
- Avoid going out when the sun’s rays are the strongest. In most areas, this is between the hours of 10 a.m. and 4 p.m., especially during the summer.
Good general care is essential. A healthy lifestyle not only improves your quality of life but may also reduce your chances of having more frequent and severe flares. Taking good general care of yourself also helps decrease the risk of heart attack and stroke. Good care includes:
- Getting vaccinations to help protect you from illnesses such as pneumonia and the flu. But some vaccinations are not safe if you have lupus. Talk to your doctor about your vaccination schedule.
- Treating high blood pressure and high cholesterol.
- Taking medicine to help prevent osteoporosis caused by corticosteroids.
- Preventing plaque in the arteries (atherosclerosis) that can be made worse by corticosteroids.
- Protecting yourself against infections you can get more easily due to decreased immune system function.
Other good health habits that will help protect you include:
- Regular exercise.
- Education about lupus and self-care.
- Not smoking. People with lupus have an increased risk of hardening of the arteries (atherosclerosis). Smoking increases this risk even more.
- A healthy, balanced diet.
- Regular dental care.
- Regular eye exams by an ophthalmologist.
- Building a support system of family, friends, and health professionals.
If you have lupus and are a woman in your childbearing years, pay special attention to pregnancy-related concerns, both before you conceive and while pregnant. Most women with well-controlled lupus can take birth control pills if they choose. And for most women, lupus won’t interfere with becoming pregnant or with pregnancy. But some women with lupus, especially those with active disease, are at higher risk of problems from pregnancy. All women of childbearing age should check with their rheumatologist when they are planning to become pregnant.
Home treatment and regular checkups are sometimes enough for managing mild lupus or for periods of remission. Be sure to have regular checkups. These checks are important to help find and treat progressive organ damage.
It is important that the people in your life understand what lupus is, how it affects your life, and how you can best cope with it. Help them understand your limitations and needs when your symptoms flare. Support groups are great places to learn coping strategies from others.
Medications
Medicines can’t cure lupus, but they can control many symptoms and often can prevent or slow organ damage.
Medicine treatment for lupus often involves reaching a balance between preventing organ damage, having an acceptable quality of life, and minimizing side effects. You will need to see your doctor often to see how you’re doing and check for medicine side effects.
Your doctor may have to change the dose and combinations of medicines until you reach the best possible balance.
Medicine choices
If you have mild disease or symptoms that affect your quality of life but you don’t have organ-threatening problems, your doctor may prescribe:
- Acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), sometimes in combination with antimalarial drugs. Acetaminophen and NSAIDS are often enough to reduce symptoms.
- Antimalarial drugs such as hydroxychloroquine (Plaquenil).
- Low-dose corticosteroids and/or corticosteroid creams or ointments.
If you have more severe disease, your doctor may prescribe:
- Corticosteroids, such as prednisone.
- Immunosuppressive medicines, such as azathioprine, belimumab, cyclophosphamide, methotrexate, or mycophenolate mofetil.
If you have had blood clots in a vein or artery (venous or arterial thrombosis), or have antiphospholipid antibody syndrome, which increases your risk for blood clots, your doctor may prescribe a blood thinner (anticoagulant). This is especially important if you already have blood clots. Aspirin is a nonsteroidal anti-inflammatory drug (NSAID) that is sometimes used to slow blood clotting in antiphospholipid antibody syndrome.
What to think about
Some lupus medicines, like acetaminophen and prednisone, are considered safe during pregnancy. Others may not be. You may not be able to stop taking lupus medicines after becoming pregnant. Or you may need to start taking medicines for a symptom flare. If possible, talk to your doctor before becoming pregnant so you can learn about the effect lupus may have on your pregnancy.
Because corticosteroids are powerful medicines and can cause serious side effects, your doctor will recommend the lowest dose that will give the most benefit.
Some people with lupus are sensitive to antibiotic medicines called sulfonamides (sulfa medicines). These include Bactrim, Septra, and many others. Your doctor can prescribe medicines that don’t contain sulfa, if needed.
People with lupus can go into spontaneous remission. If this happens to you, your doctor may cut back your medicine over time or stop your medicine.
Surgery
Surgery isn’t used to treat mild or moderate symptoms of lupus. But it may be considered for people who have permanent, life-threatening kidney damage. A kidney transplant or kidney dialysis may be done instead of continuing long-term treatment with high doses of medicines that have serious side effects.
Other Treatment
While some people with lupus try alternative or complementary therapies (such as special diets, fish oils, or chiropractic treatment), these are not proven treatments for lupus.
Some therapies that focus on relaxation can help you cope with having a long-lasting (chronic) disease and may significantly improve your quality of life. These relaxation therapies include yoga, guided imagery, and massage.
Experimental therapies for lupus
Medicines and therapies now being studied are meant to change how the immune system works so that they can keep the disease from progressing. These newer treatments include stem cell transplantation and biologic treatment.
Immunoablation with or withoutstem cell transplantation is being studied as a treatment for severe lupus that has not been controlled with all other treatments. Immunoablation uses powerful drugs to wipe out the damaged immune system. After immunoablation, either the bone marrow is allowed to replace itself, or it is partially replaced through a stem cell transplant. The transplant replaces damaged or destroyed bone marrow cells with healthy cells, or stem cells. Stem cells are immature cells that are produced in the bone marrow. They can divide to produce more stem cells. Or they can mature into red blood cells, white blood cells, and platelets. More study of these treatments for lupus is needed.
Biologic treatment blocks specific steps in the lupus autoimmune process without suppressing the entire immune system. Researchers are currently experimenting with very specific substances, such as antibodies and nucleotides, that block certain steps of the autoimmune process. Rituximab is an antibody directed against certain immune cells that may have a role in lupus. It is approved for treating rheumatoid arthritis. Studies are looking at the use of rituximab for lupus. It is beginning to be used for lupus flares that have not responded to other immunosuppressive therapies. In some cases, rituximab has been associated with serious side effects such as breathing difficulty, heart problems, or severe infection. So the use of rituximab is closely watched.
DHEA (also called prasterone in the United States) is an androgenic dietary supplement that is derived from the wild yam. Experts suggest only using pharmaceutical-grade (versus “natural”) DHEA. Results of research are mixed. But most studies show the drug has no more impact on the lupus itself than a placebo.footnote 2 The most common side effects of DHEA are acne and facial hair growth in women and hair loss in men. Because this supplement is a hormonal substance, talk to your doctor before using it. And have your DHEA blood levels checked every 6 months. Long-term effects are not known.
Plasmapheresis, the removal of some parts of the blood, is rarely used as treatment for lupus except for certain severe cases.footnote 3
Intravenous gamma globulin (IgG) may be used to treat lupus that has not responded to other treatment. There is not good evidence that this works for lupus.
References
Citations
- Petri MA, et al. (2005). Combined oral contraceptives in women with systemic lupus erythematosus. New England Journal of Medicine, 353(24): 2550–2558.
- Crosbie D, et al. (2009). Dehydroepiandrosterone for systemic lupus erythematosus (review). Cochrane Database of Systematic Reviews (4).
- Crow MK (2016). Systemic lupus erythematosus. In L Goldman, A Shafer, eds., Goldman-Cecil Medicine, 24th ed., vol. 2, pp. 1769–1777. Philadelphia: Saunders.
Credits
Current as ofApril 1, 2019
Author: Healthwise Staff
Medical Review: Anne C. Poinier, MD – Internal Medicine
Adam Husney, MD – Family Medicine
E. Gregory Thompson, MD – Internal Medicine
Martin J. Gabica, MD – Family Medicine
Kathleen Romito, MD – Family Medicine
Nancy Ann Shadick, MD, MPH – Rheumatology
Current as of: April 1, 2019
Author: Healthwise Staff
Medical Review:Anne C. Poinier, MD – Internal Medicine & Adam Husney, MD – Family Medicine & E. Gregory Thompson, MD – Internal Medicine & Martin J. Gabica, MD – Family Medicine & Kathleen Romito, MD – Family Medicine & Nancy Ann Shadick, MD, MPH – Rheumatology
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.